VAP-1 in PSC: latest findings published
New and exciting findings about the activity of the enzyme, VAP-1
Vascular Adhesion Protein-1 is elevated in Primary Sclerosing Cholangitis, is Predictive of Clinical Outcome, and Facilitates Recruitment of Gut-Tropic Lymphocytes to Liver in a Substrate-Dependent Manner
Primary sclerosing cholangitis (PSC) and inflammatory bowel disease (IBD) share an intricate relationship, although reasons as to why the two are so closely related remain elusive. Much work has gone into researching the mechanisms that drive the two diseases, and there is also evidence to suggest that IBD may also influence how the liver in PSC behaves. Emerging data from the National Institute for Health Research (NIHR) Birmingham Research Centre (BRC) provides further, novel insights in this regard. A study published in ‘Gut,’ first authored by Dr Palak Trivedi (Birmingham, UK), studies the role of a critical molecule involved in driving chronic liver disease known as vascular adhesion protein 1 (VAP-1). The study explores how VAP-1 can influence the recruitment of immune cells from the gut to the liver, but also how levels of VAP-1 that are released into the bloodstream may help identify patients with PSC at higher risk of disease progression.
It is well known that the gut and the liver express ‘adhesion molecules’ which behave as the molecular postal codes for calling specific immune cells to the respective organs. For instance, in the gut there is a molecule known as MAdCAM-1, levels of which increase during inflammation and is an important driver of IBD. Ordinarily, MAdCAM-1 is not found outside the gut, but in 1999, Professor Adams and the Birmingham group reported that MAdCAM-1 can also be found in the liver of patients with PSC; and as a result, ‘gut-derived’ immune cells would travel to, and cause inflammation within the liver. For many years, the reason for MAdCAM-1 being found in the liver of patients with PSC was unknown. However, in 2011 the Birmingham group showed that activity of an enzyme known as VAP-1 was capable of inducing MAdCAM-1 in the liver.
Dr. Trivedi’s work has followed on from this; and in the current study was able to show several new and exciting findings:
The enzyme activity of VAP-1 in the liver is dependent upon substances produced by the human body called ‘amines’. Moreover it is specific amines, particularly those known to be released by bacteria in the gut of patients with IBD as well as by the gut lining itself, which were able to activate VAP-1 to the highest degree.
VAP-1 was able to control the adhesion ('sticking') of immune cells that normally only travel to the gut, to happen in the liver.
High levels of VAP-1 are not only detected in PSC liver, but can also be released into the bloodstream. Moreover, in several hundred patients with PSC, high versus low levels of VAP-1 in blood were able to identify those who are at the greatest risk of disease progression (needing a liver transplantation or dying from their liver disease).
When asked to describe the how these results will be taken further, Dr. Trivedi said:
“Our study provides further insight into the complex interplay of gut-liver immunity in PSC, and more so identifies VAP-1 as a novel biomarker of risk for patients. We measured VAP-1 levels at random points during the clinical course of our patient cohort, and did not restrict our study to specific time points such as at diagnosis, or at 1- or 2-years etc. Despite this, we were able to show how elevated VAP-1 values in the blood identify patients having a higher chance of needing a liver transplant or dying from advanced liver disease. The next steps would be to validate these observations in patients from other centres, and also determine whether changes in VAP-1 over time are better at predicting outcome than readings at a single time point. It is also worth considering how VAP-1 levels are impacted by some of the new therapies under clinical trial, particularly as there are very few robust biomarkers of disease progression out there for patients with PSC."
The study is published in the journal ‘Gut’ and is open access meaning that you can read the article without needing to pay.
Written by Dr Palak Trivedi 08 April 2017
PSC Support funded VAP-1 research
PSC Support has funded VAP-1 research study to:
- Yield a robust, validated biomarker for patients, which is linked to the underlying disease process and accurately predicts prognosis in PSC.
- Improve understanding of the features that define high versus lower risk groups.
- Provide a better evidence base to identify those most in need of new treatments, and consequently refine the criteria that determine clinical trial eligibility.
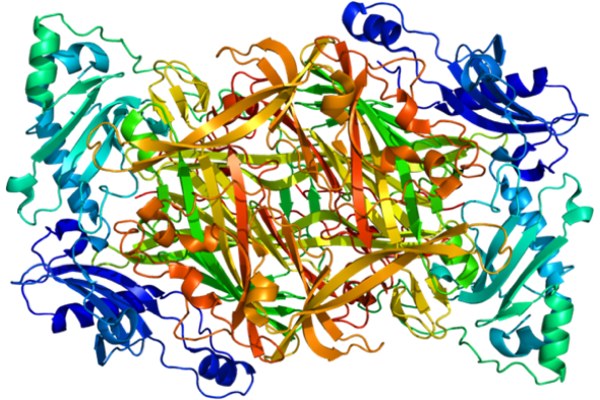
Image courtesy of EMW: CC BY-SA 3.0 Protein AOC3 PDB 1pu4
Trivedi PJ, Tickle J, Vesterhus MN, et al Vascular adhesion protein-1 is elevated in primary sclerosing cholangitis, is predictive of clinical outcome and facilitates recruitment of gut-tropic lymphocytes to liver in a substrate-dependent manner Gut Published Online First: 20 April 2017. doi: 10.1136/gutjnl-2016-312354
