Working with your doctor
It is essential you are monitored when you have PSC, even if you are asymptomatic (have no symptoms). Therefore, expect to be monitored on ongoing basis by your GP and PSC/IBD doctors over your lifetime.
As time passes, you’re likely to become an expert on your condition, and may feel able to work closely with your medical team to get the right care for you.
Who is my PSC doctor?
Your PSC doctor might be a hepatologist or a gastroenterologist. Often, PSC is diagnosed following routine IBD tests, and many people with PSC continue to see their gastroenterologist for their IBD (if they have it) and also for their PSC. If your PSC is asymptomatic and stable, this is a sensible choice. If your symptoms are progressing, then a PSC specialist might be a more suitable option. If you do need to see a PSC specialist, there is no reason not to continue to see your IBD doctor for IBD (if you have IBD). Colonoscopies at your local hospital are easier logistically!
How often should I see my PSC doctor?
Your PSC doctor will arrange to see you at regular intervals, depending on your individual needs. Some asymptomatic patients see their PSC doctor every 12 months (with a blood test at their GP’s every 6 months), while others require more frequent monitoring.
If you are concerned about a change or development in your condition before your next scheduled appointment, get in touch with your PSC doctor. It can be helpful to keep track with a diary of how you feel and function, and do take notice if friends and family notice something you haven’t!
How can I get in touch with my PSC doctor?
Most hospitals provide details of how to get in touch with their service in their letters to you. However, these letters can take weeks to arrive. We suggest you ask your doctor during your appointment how to contact them if you are concerned about symptoms once at home.
What kind of monitoring will I have?
Once you know you have PSC, you may wish to consider finding a PSC specialist. You are entitled to ask for a referral for specialist treatment on the NHS. Generally speaking, if your PSC is asymptomatic (has no symptoms) and stable, you can be seen in a general clinic 58. If your PSC is complex or symptomatic, talk to your doctor about being referred to a hospital with PSC expertise /conducts PSC research. However, whether you will get the referral depends on what your GP feels is clinically necessary in your case.
The BSG/UK-PSC Guidelines58 recommend that ‘patients with symptomatic, evolving or complex disease should be referred for expert multidisciplinary assessment.'
If there is doubt about your PSC diagnosis, we recommend referral for specialist opinion.
What will my GP do?
PSC is rare and most GPs will be unfamiliar with the disease. It’s not realistic to expect your GP to be an expert on PSC - you may be the only PSC patient at your GP’s practice! What you can do, is work with both your GP and your PSC doctor to learn how to manage PSC and any symptoms.
Preparing for your appointment
It’s a good idea to prepare yourself for your hospital appointment to ensure you get the most out of it.
As hospital systems restart following the COVID-19 pandemic, you may find that some of your appointments are 'virtual', meaning they take place with video conferencing or by telephone. Others may take place in a different hospital to usual, or you may see a different doctor. It's important to have all the information you need to hand so you can make the most of those moments with your PSC doctor or nurse.
Think about what you want to tell your doctor, and what you want to ask in advance. Because there is limited time in clinics, it is unlikely that your doctor will be able to answer all your questions. Take a look at the following list of questions to help you identify the most important questions you want to ask and pick your top three.
Questions for your PSC doctor
Communication
- How can I contact you if I have concerns that I think relate to my PSC in office hours and out of office hours?
- Ensure doctor/nurse has your correct contact details including phone number.
Symptom Issues
- What symptoms should I watch out for and what should I do if they occur?
- I have *this* symptom. What does it mean?
- I have *this* symptom. How can it be managed or treated?
- I think my IBD is flaring *here’s how*. How can it be managed or treated?
Management of PSC
- Is my PSC stable? If not, what are the next steps?
- How often will I need to see you for my routine care?
- What routine tests do I need now and how often?
- Can I arrange to get blood tests done locally in advance so we can discuss the results?
- What do my test results mean?
- I have never had a bone density scan (DEXA scan). Do I need one?
- I have never had a colonoscopy. Do I need one?
- I have never had an ultrasound scan. Do I need one?
I have never had an MRI scan. Do I need one? - I have recently had bacterial cholangitis, how will this be followed up?
- I needed to go to hospital/seek urgent care for a PSC/liver issue since I last saw you. Do you need to follow-up?
Medication
- What is the medication trying to achieve?
- What are the side effects of my medication?
- Can you review my medications?
- What pain relief am I allowed to take?
PSC Research
- Am I eligible to go on any current clinical trials (or PSC research in this hospital)?
- Can I give a UK-PSC blood sample?
Living with PSC
- Do I need any vaccinations? (flu, hepatitis A and B, pneumococcal vaccine)
- Can I have occasional alcohol/ low alcohol?
- Are there any lifestyle/dietary changes I should make?
- Will liver disease affect my ability to work?
- Can I travel abroad?
Resources to live better with PSC
Royal Free Question Prompt List
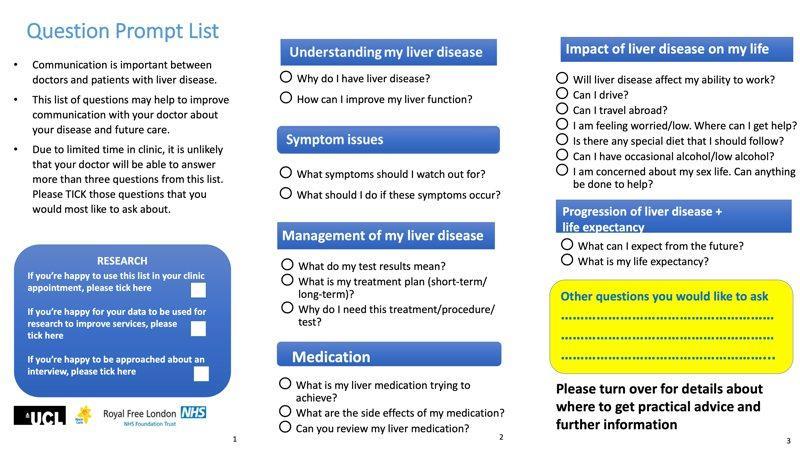
Researchers have developed a set of questions and prompts that can be used to improve communication in appointments138.
View the prompts by clicking the images below or download the pdf to print out:
NHS urgent care near you
As with any disease, there may be times when you need to seek urgent medical advice (see when to contact your PSC doctor).
If you need help straight away, but it isn’t an emergency, call 111 (excluding Northern Ireland). Northern Ireland (out of hours numbers)
Out of hours care
Familiarise yourself with your GP’s out of hours procedures. It’s funny how often the time you need to speak to someone is at 8am on a Sunday morning!
Remember it is not realistic to expect any GP to have vast experience and knowledge about PSC.
It can be very useful to have a letter from your PSC doctor which explains that you have PSC, what medication if any you are taking, and what medication you can/can’t have.
England (location search for urgent care)
Northern Ireland (out of hours numbers)
Wales (GP out of hours numbers)
If you suspect you have a bile duct infection, and need antibiotics urgently, print off our Bacterial Cholangitis leaflet to support decision-making.
Remember, PSC is rare so it helps everyone if you can show them evidence-based facts about PSC.
If you want to make an appointment to see your GP about a suspected bile duct infection, you should ask for an emergency appointment, not a routine one, and be clear: ask to see seen that day if possible because you think you have a bile duct infection.
People with PSC often have other diseases and might therefore need a number of prescriptions. You are responsible for ensuring that you understand why you are taking the medication prescribed to you. If you are unsure, ask your doctor or nurse to explain. You should also have your prescriptions reviewed on a regular basis by your GP or pharmacist.
If you are at all concerned about your health and suspect that the issue is related to PSC, let your doctor know. It’s important to know when to contact your doctor. Click here to find out more: