Liver Transplant Services in the UK
Survey report
Download full report
Wider, longer-term services needed for liver transplant patients
In February 2020, we conducted a survey to find out what sort of care is important to people having liver transplants. We found important gaps in service provision and PSC Support is working with leading transplant clinicians to improve services for patients before and after liver transplant.
We’re using these results to help demonstrate the urgent need for wider services and support for liver patients before and after transplant.
Liver Transplant Services Survey
Download Full Report
 Recommendations
Recommendations
- Transplant units must be equipped to enable people:
- who are waiting for transplants to be as fit and psychologically ready as possible for not just the operation, but life after it.
- who have had transplants to feel prepared physically and mentally to resume everyday activities, including work and education.
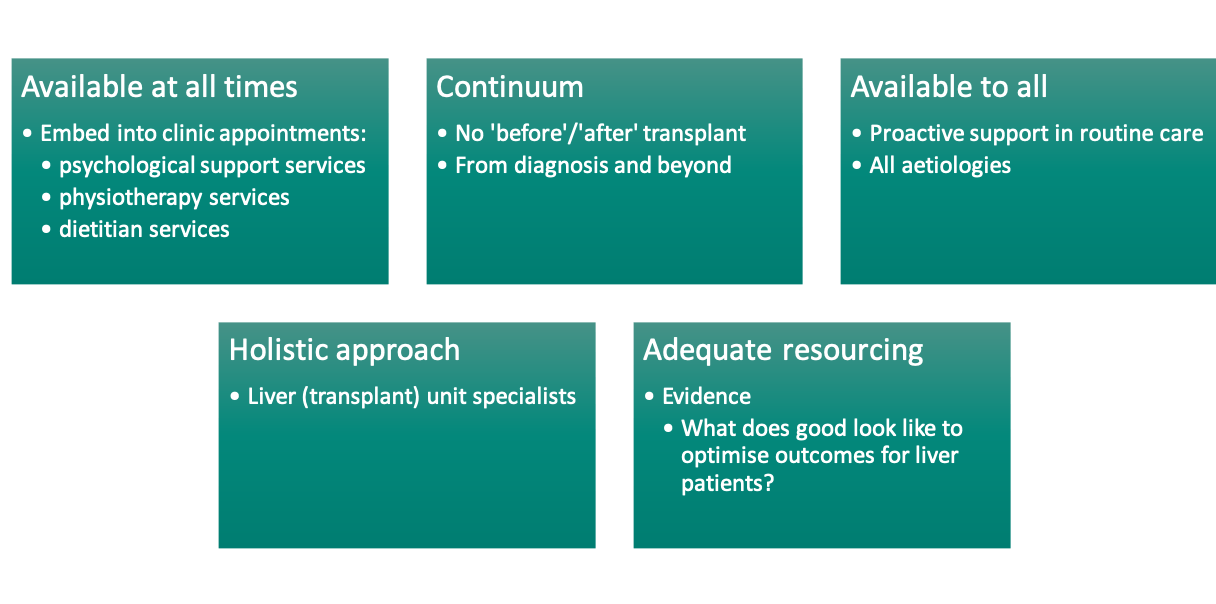
- We believe that the following standards are critical for patients from the time of transplant assessment and continuing into the long term post-transplant:
- Specialist psychological support services, physiotherapy services and dietitian services are embedded into liver transplant services for all patients, regardless of transplant indication or stage in their transplant journey.
- Patients are proactively asked about wellbeing and supported through physiotherapy, dietician and psychotherapy services.
- Quality of life is evaluated and acted upon using appropriate tools and interventions.
- General patient guidance from liver transplant units is consistent.
- Psychological support services, physiotherapy services and dietitian services should be available for liver disease patients in all liver units, regardless of aetiology or stage of disease.
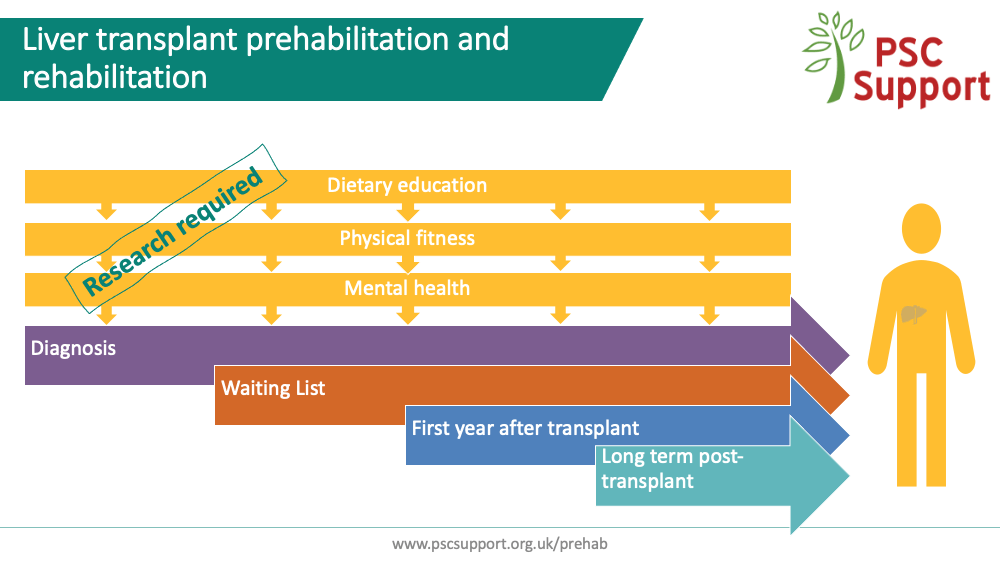
- Research is urgently needed to understand the impact of interventions to improve physical fitness, dietary education, and mental health and wellbeing so that appropriate care can be provided for liver disease patients to optimise outcomes for all.
- Liver transplant units should be adequately resourced to be able to provide these services.
There is no doubt that excellent support and advice before and after liver transplant in the UK is available, but this is not universal. Comments from survey respondents praised staff in transplant units for their dedication and efforts for patients.
The recently introduced Liver Transplant Offering Scheme is based on the principle that donor organs are placed according to greatest ‘transplant benefit’. This integrates elements of a patient’s need for a transplant and a patient’s utility from receiving a particular donated liver. Strictly speaking, the intention is to maximise life-years gained from transplanting a donor organ, but in an era where quality of life matters, how well patients live is crucial too.
The 2017 Service Specification for Liver Transplantation Service in Adults states that, ”A transplant also offers the opportunity for an improved quality of life and greater social independence. Transplantation is not only beneficial for the individual but also represents value to the greater health economy. In addition, some patients can return to work and therefore have a lower dependency on state support.”
However, the service specification has a focus on particular timepoints in transplantation e.g. when making an informed choice about having the transplant, “Support from Clinical Psychology should be offered to meet the needs of patients”.
Whilst specialist services (e.g. dietician, pharmacist, physiotherapist, psychiatric liaison nurse) are specifically mentioned within the document, and as a minimum, patients can expect to have access to “all members of the multidisciplinary team to discuss specific problems or concerns”, this does not go far enough. These services should be available as standard for all patients from the time of transplant assessment in order to proactively optimise wellbeing and outcomes for patients, and not be available only when problems or concerns arise. There should be a greater emphasis on the holistic, long-term care of patients from the moment they are assessed for transplant.
The progression of some liver diseases can be halted or reversed with healthy lifestyle modifications and may result in improved outcomes overall and a reduction in numbers referred for transplantation, and consequent demand for donor organs. For this reason, we believe that psychological support services, physiotherapy services and dietitian services should be available for liver disease patients in all liver units, regardless of aetiology or stage of disease. Liver disease is rarely solely about the liver, and patients should be treated holistically from the outset.
However, we are concerned that transplant units are not properly resourced to be able to provide all the specialist services that people need at times they need them. In addition, evidence demonstrating what optimal, holistic care should look like is lacking. There is an urgent need to clearly understand this.
- Nearly three quarters of respondents said that psychological support was very or extremely important while on the waiting list (75%) and during the first twelve months after transplant (72%).
- Anxiety was experienced by 54% of people on the waiting list, 52% during the first year after transplant and 35% after the first year post-transplant.
- Seven out of ten (69%) people on the waiting list for a liver transplant indicated that they needed psychological support.
- 58% of people who had had a transplant in the previous twelve months indicated that they needed psychological support at this time.
- 84% post-transplant patients said that physical fitness advice was very or extremely important during the first twelve months after transplant.
- Two out of every three (65%) people who had had a transplant didn't know what intensity of exercise was safe or what kind of exercise was safe (63%) during the first year after transplant.
- Two thirds (69%) of people who were on the waiting list said they needed help to stay fit enough for transplant while on the waiting list.
- Three-quarters (75%) said they needed help during the first year after their transplant to regain a good level of fitness.
- Most said specific dietary advice (83%) was extremely or very important while on the waiting list (83%) and during the first year after transplant (85%).
- A third (32%) of those who had had a transplant said they felt pressured to return to work. Two out of three cited financial reasons (67%) and pressure from themselves (61%) for returning to work before being physically and mentally ready.
"Lack of psychological support is my major take away. A transplant is a massive thing to come to terms with and the mental side of things is currently neglected.”
"Nobody seems to know how to advise people who want to be really fit and active post transplant. All the advice is tailored to the old and sick and I felt I had to make it up as I went along."
“I definitely feel there needs to be more psychological help immediately after and within the first year of transplant, as personally I found this time the most difficult and did not have any care in this area."
“Abandoned after leaving hospital after transplant....had to find support and do own research"
“I think it is very difficult when you live so far away from your transplant unit to get any day to day week to week support. More robust liaising with local services would be good"
"I can not fault the care and attention I received from all of the medical team as regards my actual transplant, but I was totally unprepared for the feelings and emotions I was to experience post transplant and I don't think I ever will be totally over them, and I honestly believe that more should have been done to prepare me for those feelings."
“I got very limited advice mainly from physio in hospital. I went to a rehab physio privately and then to a personal trainer afterwards which was good but they were unclear themselves what a post Tx person should do”
“I’m still in my first year of recovery and I want to exercise as I know my physical activity isn’t what it was pre-transplant but I don’t know how to go about it, or how intense to go. I don’t want to accidentally overwork myself and cause a hernia or some further health problem.”
“Things were offered very early on but actually, I needed support emotionally and psychologically about 6 months post”
“The dietary support I received was exceptional. As the NAFLD progressed I was monitored closely and dietary changes made to help me. After the Op I was given encouragement and support to again readjust diet.”
“Each hospital has different dietary restrictions, this should be standardised”
“After my transplant i gained a lot of weight and struggled to get back to a health weight.”
PSC Support developed the questions with support from British Liver Transplant Group clinicians and LIVErNORTH. Using an online survey, we asked people for their views on care while on the waiting list for a transplant, during the first twelve months after transplant and in the longer term. We invited people to take part by sharing the survey through our social media channels, and, to ensure that as many indications for liver transplant were included as possible, the Liver Patients' Transplant Consortium (LPTC), LIVErNORTH and the British Liver Trust also shared the survey.
We asked questions about four topics:
- psychological issues and support
- physical fitness issues and support
- dietary issues and support
- starting or returning to work/education after liver transplant
The survey ran for 14 days (10 to 24 February 2020).
436 people started the survey. 425 were from the United Kingdom. For the purposes of improving liver transplant services in the UK, only UK results are shown in this report.
407 people from the UK answered the demographics questions of which 259 went on to answer the topic questions. Only the responses from 259 people from the UK who answered topic questions are included in this report. Including data from those who only answered the demographic questions would misrepresent the backgrounds of those who went on to answer the topic questions.
Thank you to everyone who completed the survey.
While this report does not include everyone's answers, rest assured that everyone's responses have been reviewed and are being used in our advocacy work to improve liver services overall. We are grateful for the time people have given in sharing their important views.
Respondents' ages ranged from under 18 to over 65 years old.
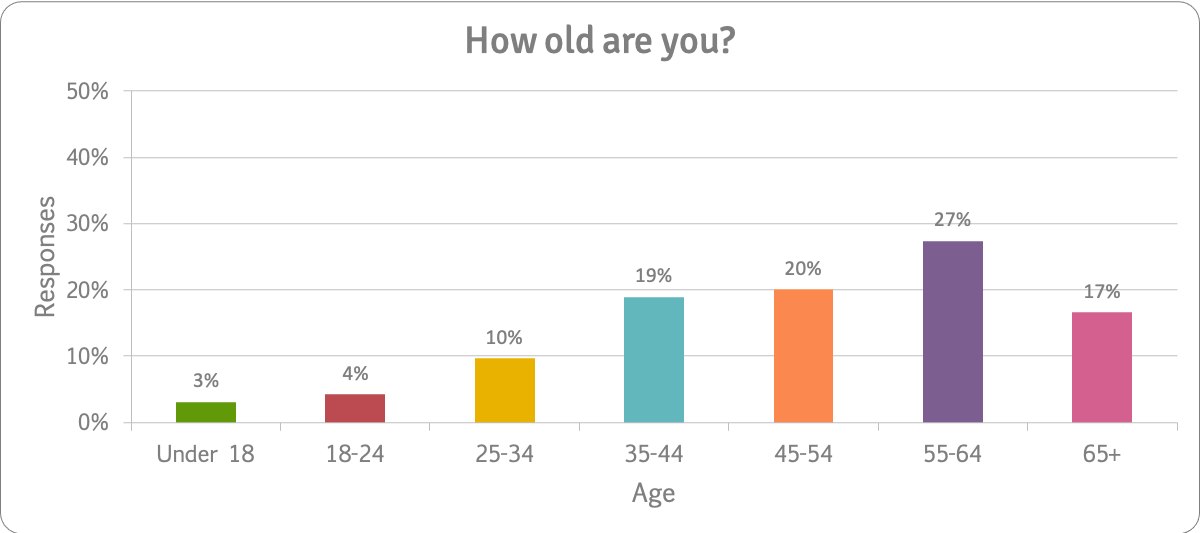
259 people answered this question.
We asked people how many liver transplants they had had and when. Most (64%) had had one liver transplant over a year ago:
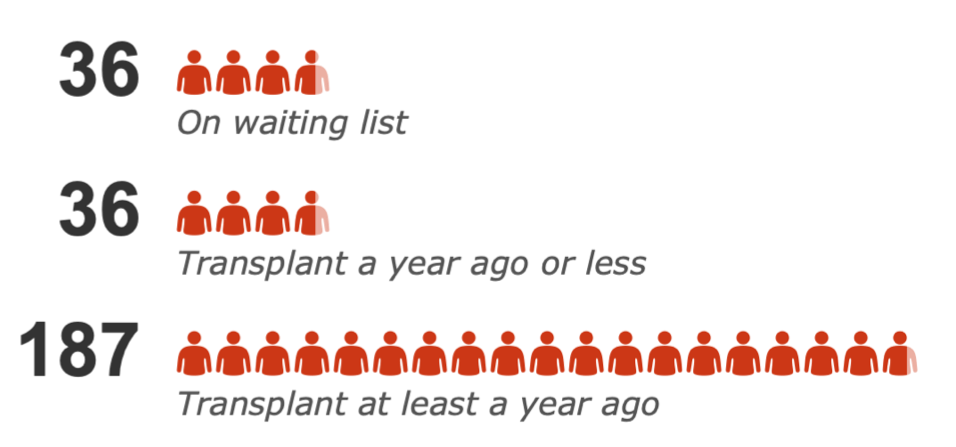
- 36 (14%) people were on the waiting list for a transplant.
- 36 (14%) had had a transplant less than a year ago.
- 187 (72%) had had a transplant at least a year ago or had had more than one transplant.
We asked people in what year they had had their transplant.
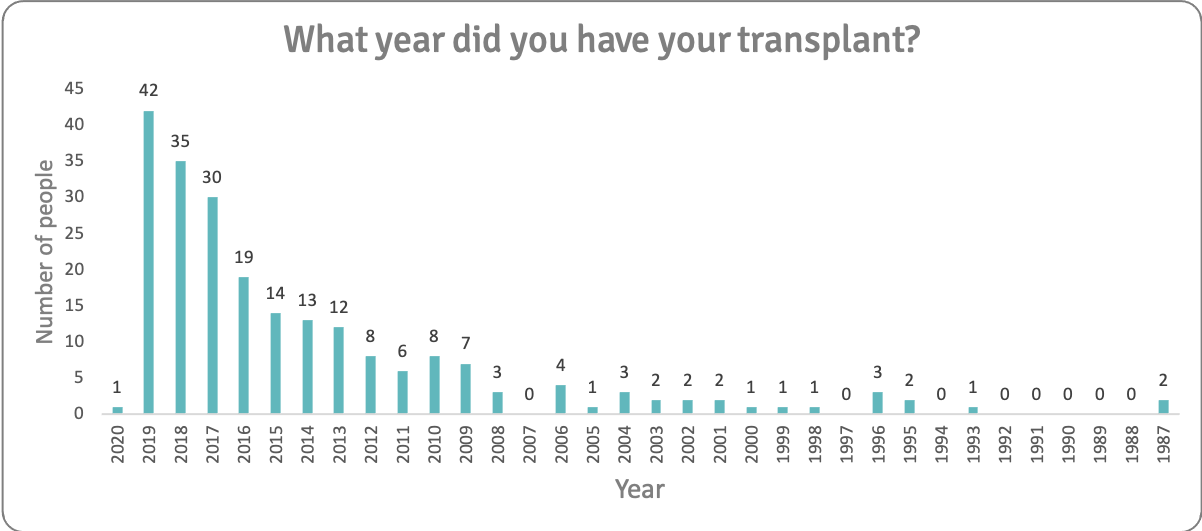
43 people had had their transplant in 2019 or 2020. Two people had had transplants 33 years ago, in 1987. Although we did not collect IP addresses (to protect respondents' privacy), their individual responses were sufficiently different for us to believe that this was indeed two separate people.
223 people answered this question.
People with a broad range of liver conditions took part.
The survey was shared in the Liver Patients' Transplant Consortium network, by the British Liver Trust, LIVErNORTH and on online support groups for transplant patients. The Queen Elizabeth Hospital (Birmingham) shared the survey during clinic time.
The high proportion of PSC patients reflects the high engagement of people in this patient group.
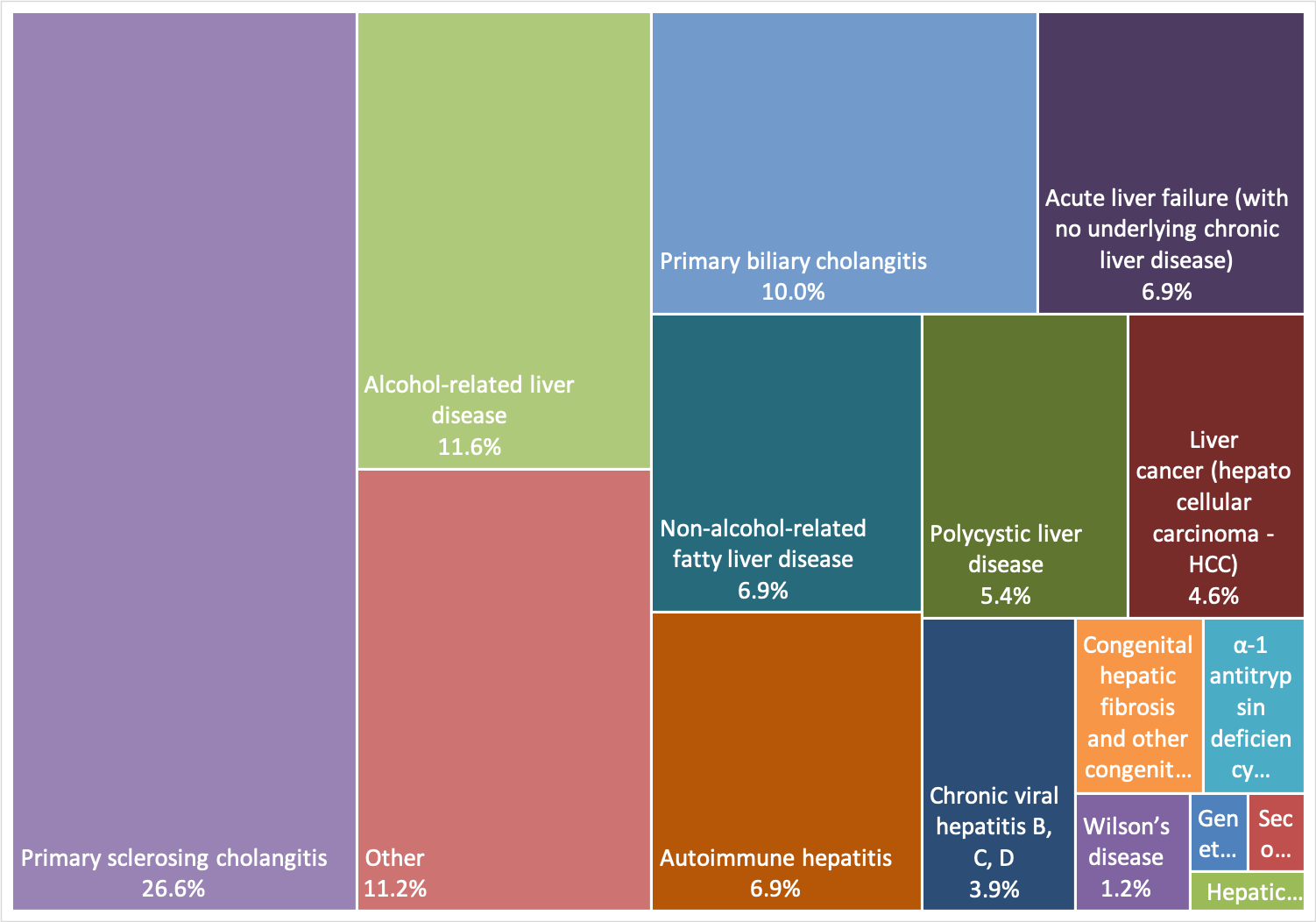
259 people answered this question.
| Condition | Count | % |
| Acute liver failure (with no underlying chronic liver disease) | 18 | 7% |
| Alcohol-related liver disease | 30 | 12% |
| Autoimmune hepatitis | 18 | 7% |
| Chronic viral hepatitis B, C, D | 10 | 4% |
| Congenital hepatic fibrosis and other congenital or hereditary liver diseases | 5 | 2% |
| Familial amyloid polyneuropathy | 0 | 0% |
| Familial hypercholesterolaemia | 0 | 0% |
| Genetic haemochromatosis | 1 | 0% |
| Hepatic epithelioid haemangioendothelioma | 1 | 0% |
| Liver cancer (hepatocellular carcinoma - HCC) | 12 | 5% |
| Non-alcohol-related fatty liver disease | 18 | 7% |
| Other | 29 | 11% |
| Polycystic liver disease | 14 | 5% |
| Primary biliary cholangitis | 26 | 10% |
| Primary sclerosing cholangitis | 69 | 27% |
| Secondary sclerosing cholangitis | 1 | 0% |
| Wilson’s disease | 3 | 1% |
| α-1 antitrypsin deficiency | 4 | 2% |
Respondents reported complications before transplant. The most commonly reported complications were ascites (fluid in the abdomen) and itch. This was a difficult question for patients to answer, and they reported many additional complications including jaundice, nausea, weight loss, varices, pain and fatigue.
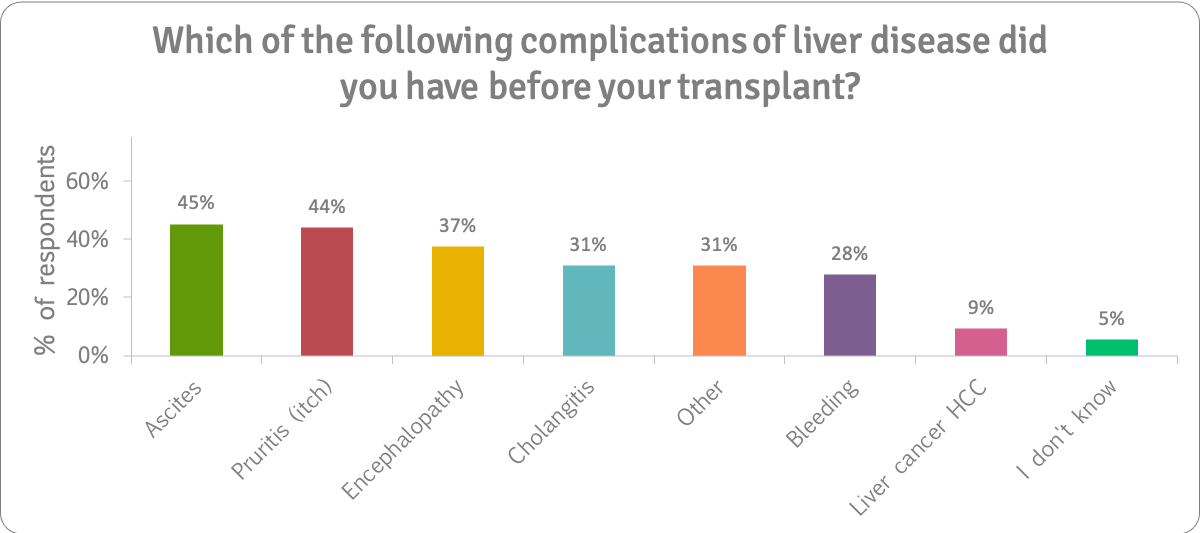
259 people answered this question.
We asked how many months people had waited for their liver transplant.
The chart below shows the number of months people who were still on the waiting list had been waiting. Nearly half had been waiting for three months or less:
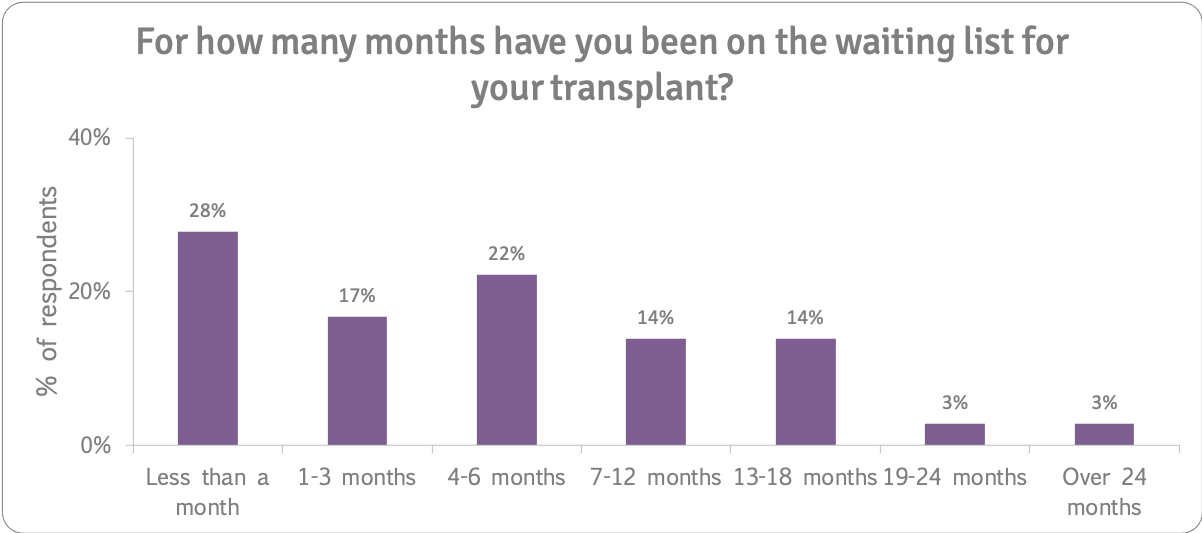
33 people answered this question.
The chart below shows the number of months people who had had a transplant were on the waiting list. Nearly half waited up to three months for their transplant:
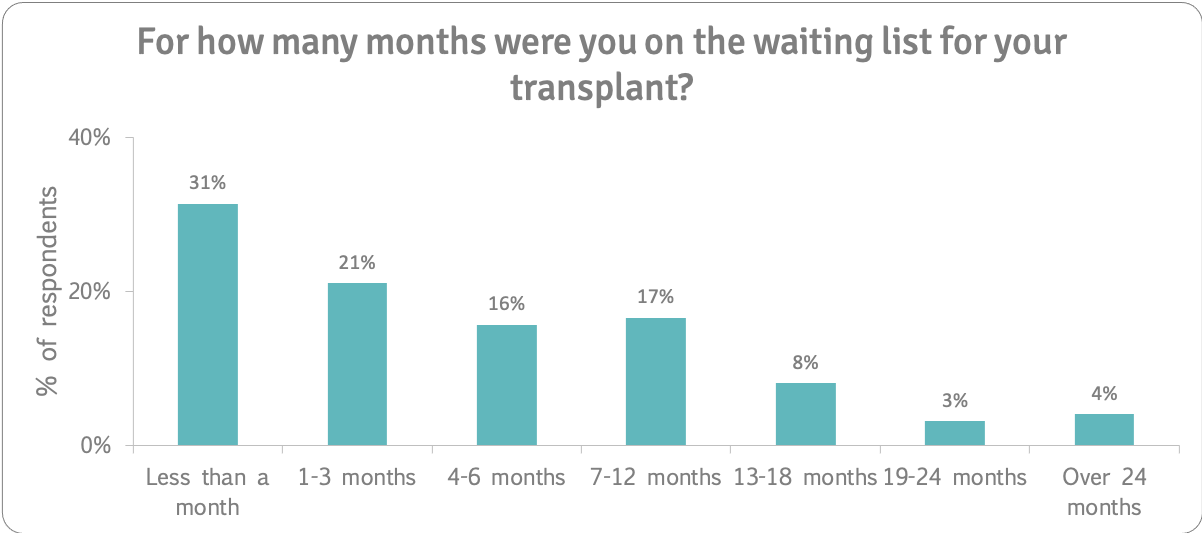
223 people answered this question.
The graph shows how many days people spent in hospital for their liver transplant.
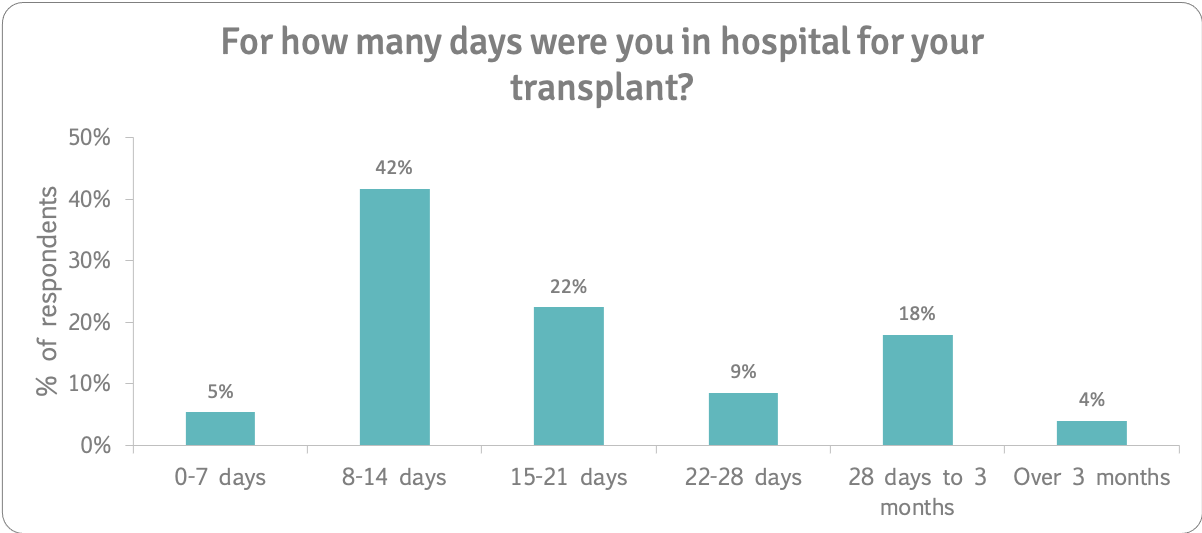
The number of days spent in hospital varied. 42% spent 8-14 days in hospital for their transplant. Around two-thirds of people who had had transplants spent three weeks or less in hospital.
223 people answered this question. Only people who had had a transplant were asked this question.
We asked respondents how important it was to be given psychological support before and after transplant. Overall, nearly three quarters of our respondents said that psychological support was very or extremely important while on the waiting list (75%) and during the first twelve months after transplant (72%). Half said it was extremely important. A quarter felt it was extremely important after the first year of transplant too.
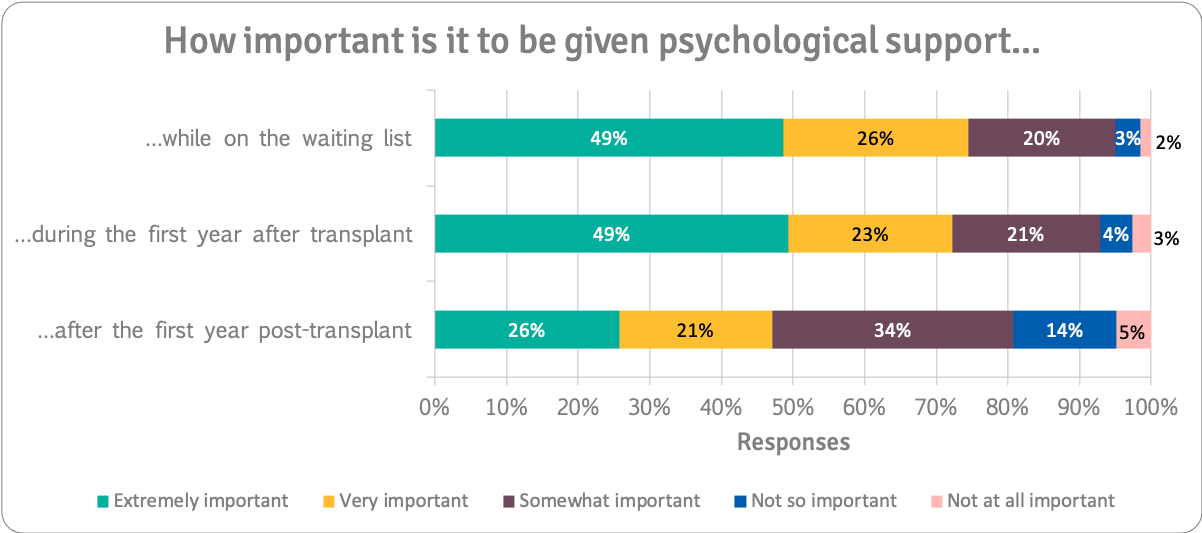
259 people answered this question.
However, the importance of psychological support is highest to people who are on the waiting list. The chart below shows responses from the 36 people who were on the waiting list at the time of the survey. 67% felt that psychological support was extremely important.
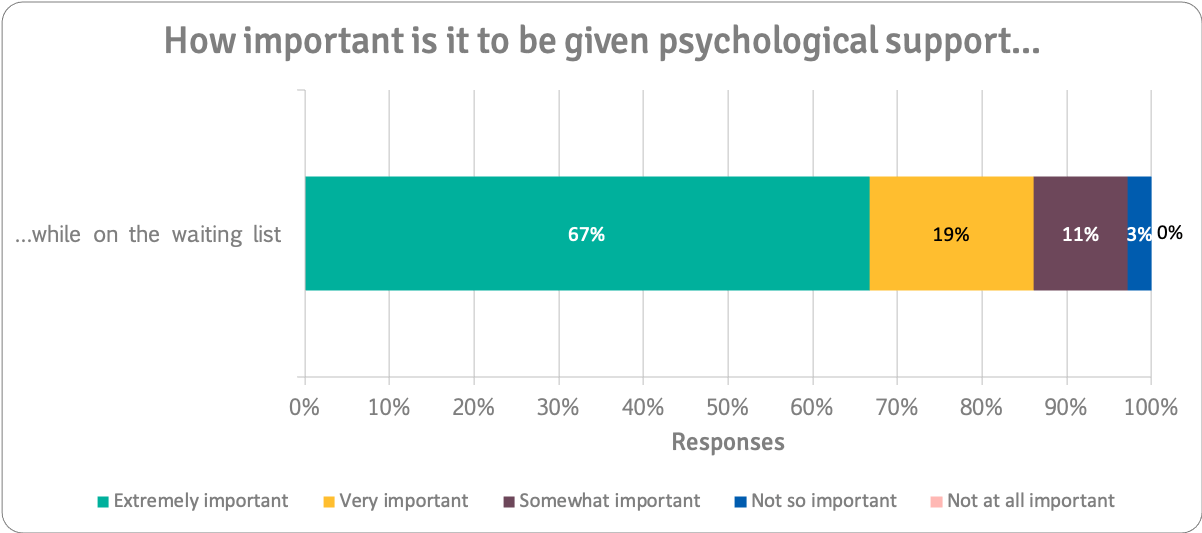
36 people answered this question.
While on the Waiting List
We asked respondents to tell us about psychological issues they were experiencing (if on the transplant list at the time) or which they had experienced while on the transplant list. Over half (54%) identified anxiety, and 37% identified stress and depression/low mood (37%) as issues. Other issues included feeling isolated, feeling guilty, and feeling overwhelmed. You can see the percentage of people that picked each issue on the chart:
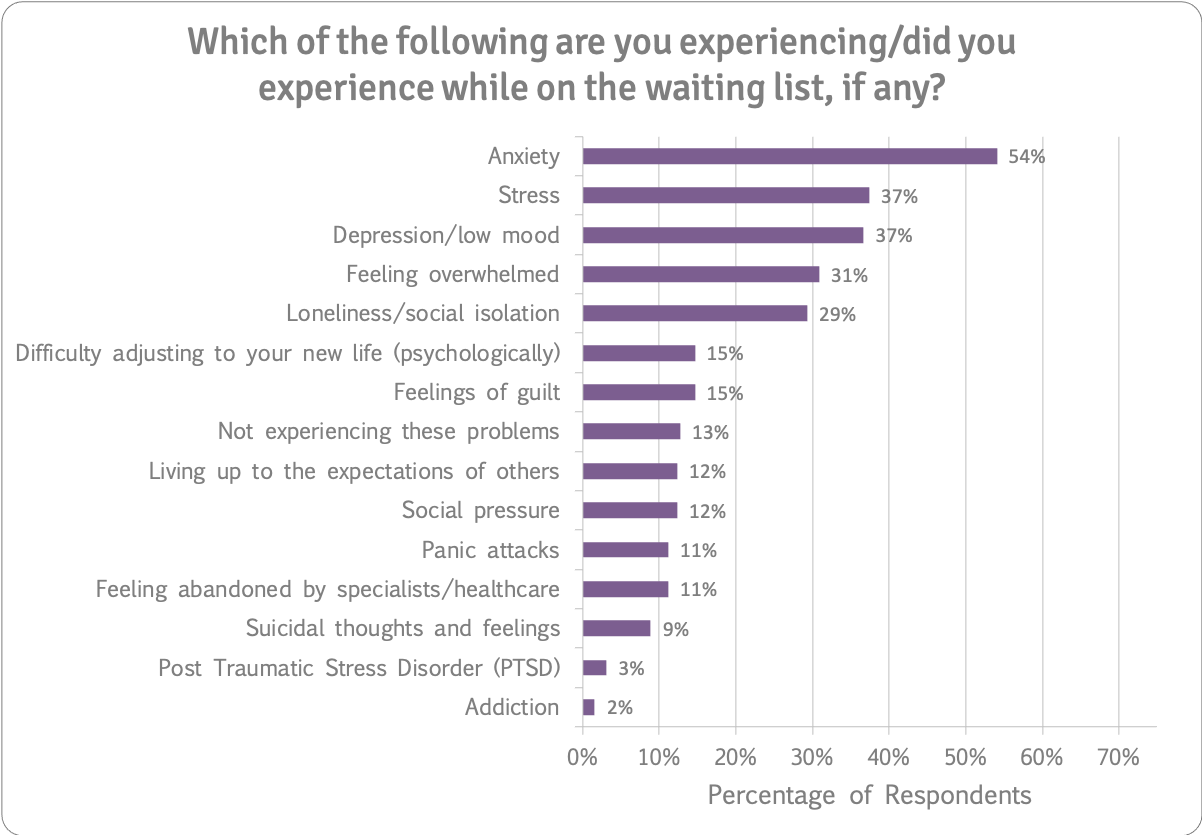
259 people answered this question.
During the First Year After Transplant
During the first year after transplant, respondents indicated that they experienced anxiety (52%), feeling overwhelmed (48%), depression/low mood (44%), stress (44%), difficulty adjusting to their new life (43%), and feelings of guilt (41%), among numerous other thoughts and feelings:
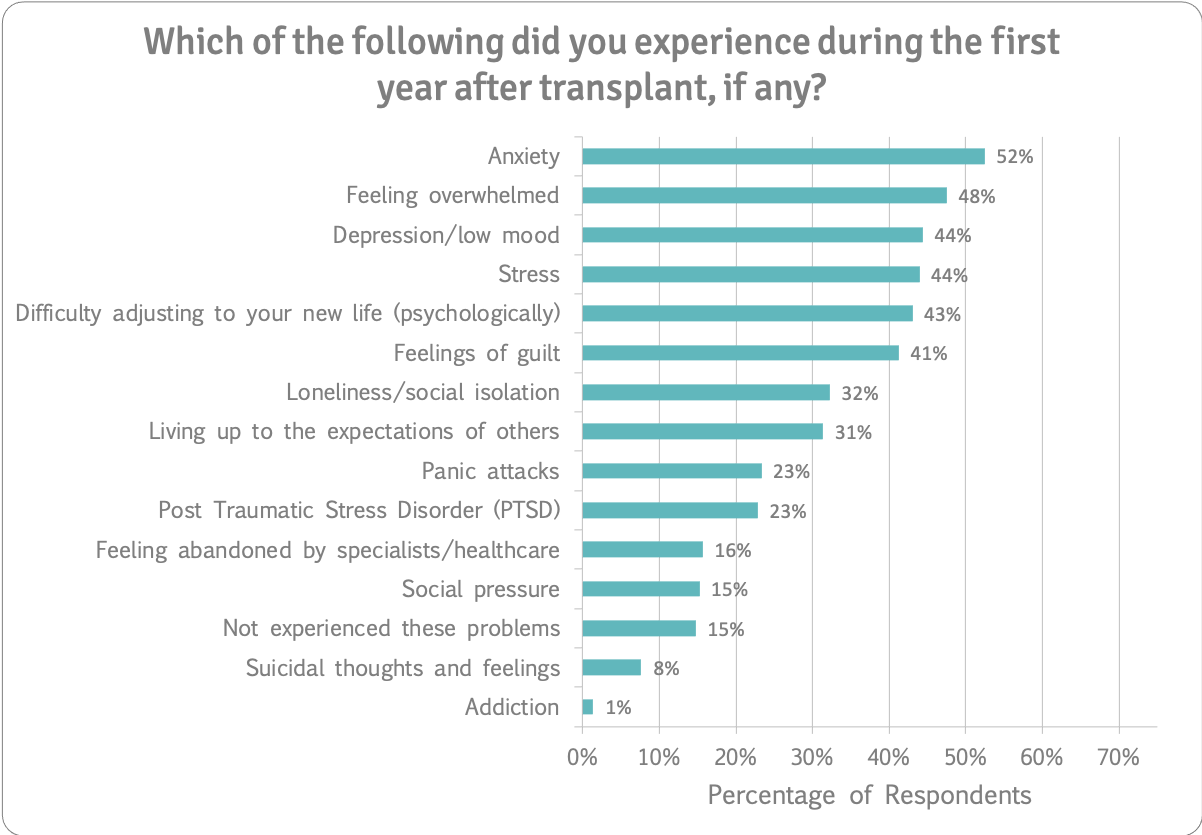
223 people answered this question.
After the First Year Post-Transplant
We asked people who had had a transplant at least a year ago what psychological issues they experienced after that first year. Anxiety (35%), depression/low mood (34%), stress (30%), feeling overwhelmed (29%), difficulty adjusting to new life (28%), feelings of guilt (28%) and living up to the expectations of others (28%) were the most frequently reported issues.
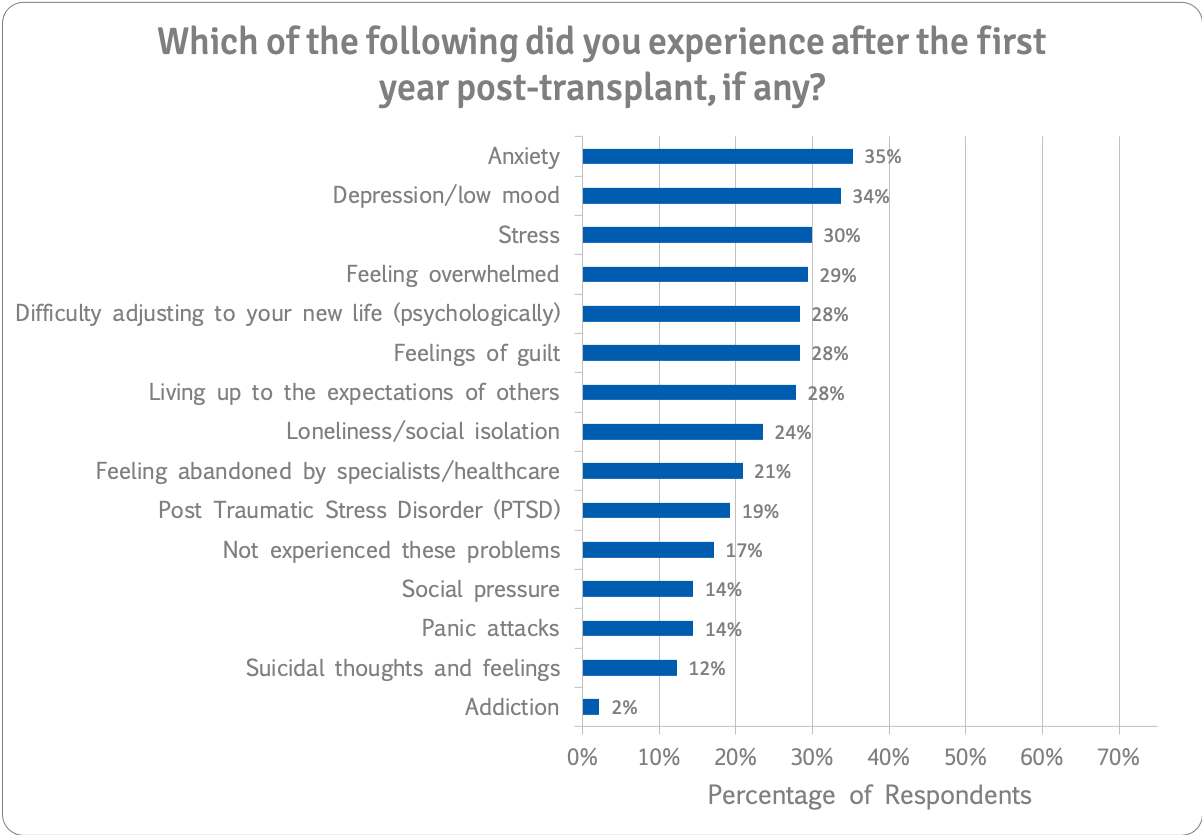
187 people answered this question.
Support On the Waiting List
We asked people if they felt they needed psychological support while on the waiting list. This chart displays what each group of people said:
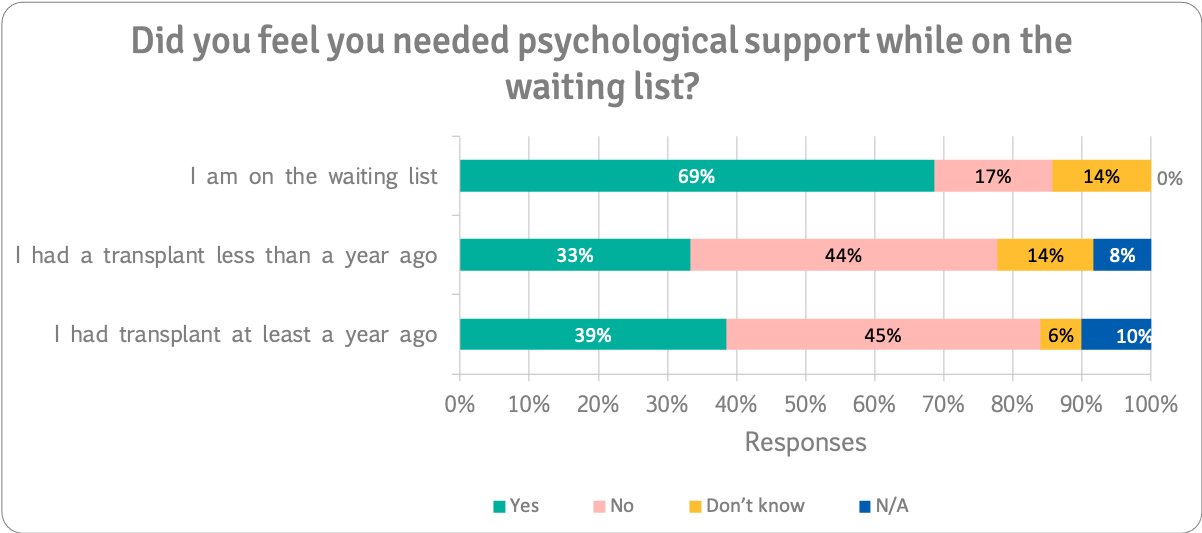
People who were actually on the waiting list at the time of the survey were more likely to say that they needed support while on the waiting list (69%) than those who had already had transplants who were looking back on their time on the waiting list (33-39%).
259 people answered this question.
Support During the First Year After Transplant
We asked respondents if they felt they needed psychological support during the first year after transplant. This chart displays what each group of people said. Note that the people on the waiting list were not asked this question:
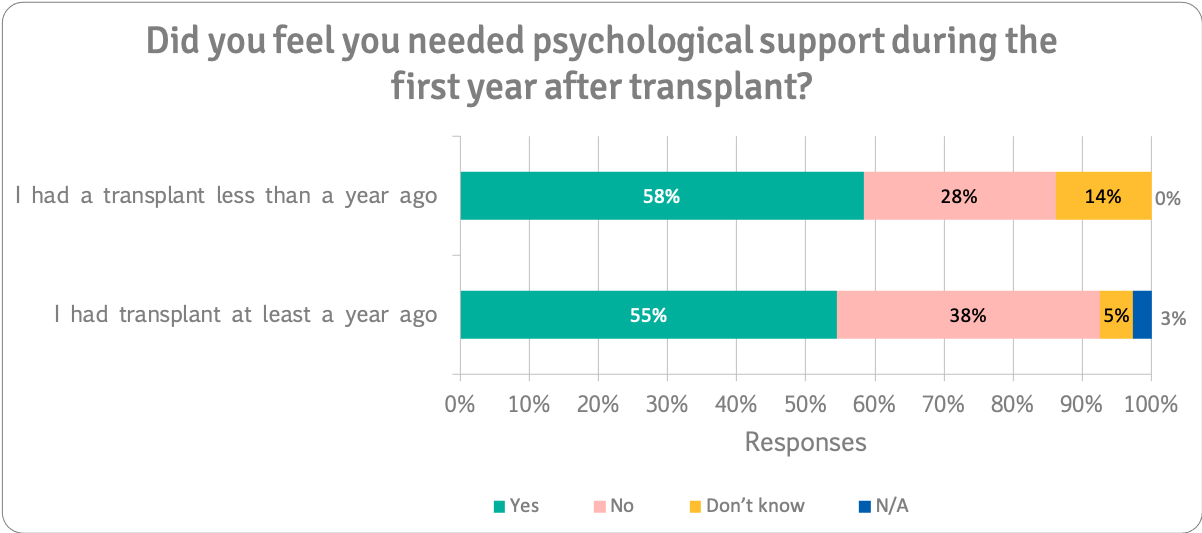
Over half of the respondents indicated that they needed psychological support after their transplant.
223 people answered this question.
Support After the First Year Post-Transplant
We asked respondents if they felt they needed psychological support after the first year post-transplant. This chart displays what each group of people said. Note that the people on the waiting list and people who had a transplant within the last 12 months were not asked this question:
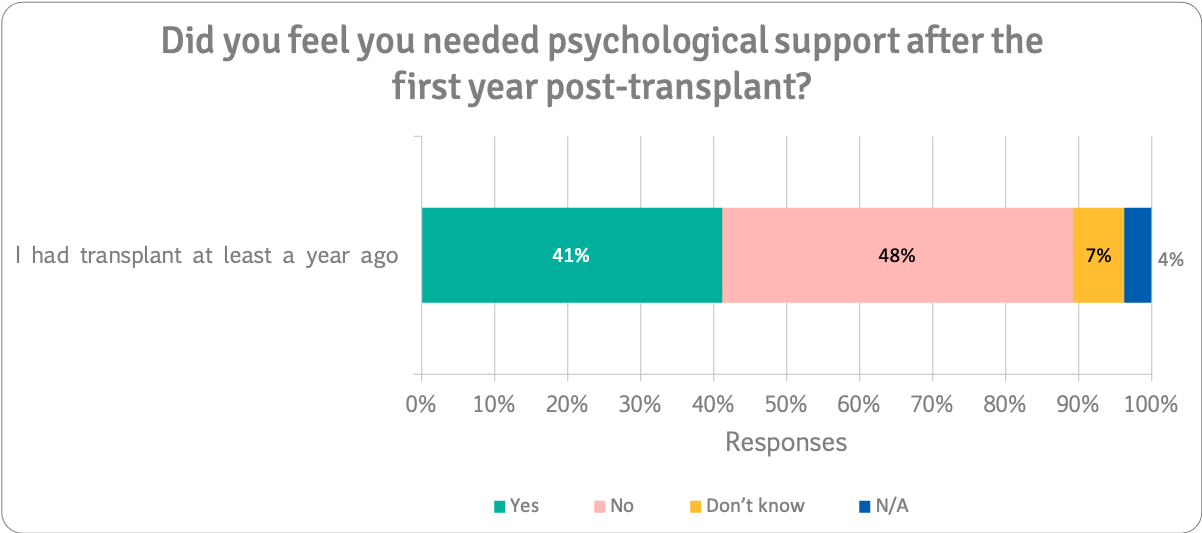
Although half (48%) said they did not need psychological support after transplant, 41% said they did.
187 people answered this question.
On the Waiting List
“I sought support whilst on the waiting list, my transplant centre didn't offer this service. I suffered anxiety & depression & was struggling to come to terms with an uncertain future. I would have benefited more if I had talked to a health professional who was familiar with liver disease and the transplant process”
“Uncertainty of what the future will bring / look like.”
“I am already receiving the relevant support from a designated psychologist”
During the First Year After Transplant
“I had a massive psychotic episode and no-one recognised what was happening or how to manage it. I was considered 'over-anxious'. I ended up very unwell pscyhologically. It possibly was avoidable with better psychologcal provision within the tranplant service [sic]”
“Things were offered very early on but actually, I needed support emotionally and psychologically about 6 months post”
“You're so ill pre transplant that you just want the operation. Post op when you're in the early stages of recovery you are laid up and have a lot of time to think, you begin to process what you went through on the waiting list. When you were so busy trying to deal with your illness physically, you had little time to devote to the physiological impact”
After the First Year Post-Transplant
“Only much later did I start to think about how close I came to dying. Subsequently I felt guilt, not about my donor, but about close friends who have not survived their illnesses. Why did I?”
“PTSD and other mental health issues have been more prevalent post-transplant. It creeps up on you. There's also constant pressure to live a ‘full life’ & be happy for the gift of life so if you do feel down you feel guilty for doing so”
“I am a positive person and didn't need phycological [sic] help pre or post, I had an excellent recovery, and was back to normal by 4 months post, didn't feel like I needed help”
“I did not seek psychological support as I felt it was my responsibility to sort myself out with the help of my family. Probably should of [sic] sought support but that is not me”
Beneficial Psychological Support
We asked respondents what kind of psychological support they would find helpful before and after transplant.
We asked people to choose three types of psychological support that they thought would be most beneficial while on the waiting list. The charts below show the percentage of respondents who picked each type of support.
Having a mentor or buddy while on the transplant list was most often preferred (40% of respondents), closely followed by face to face individual support from a mental health professional (37%)
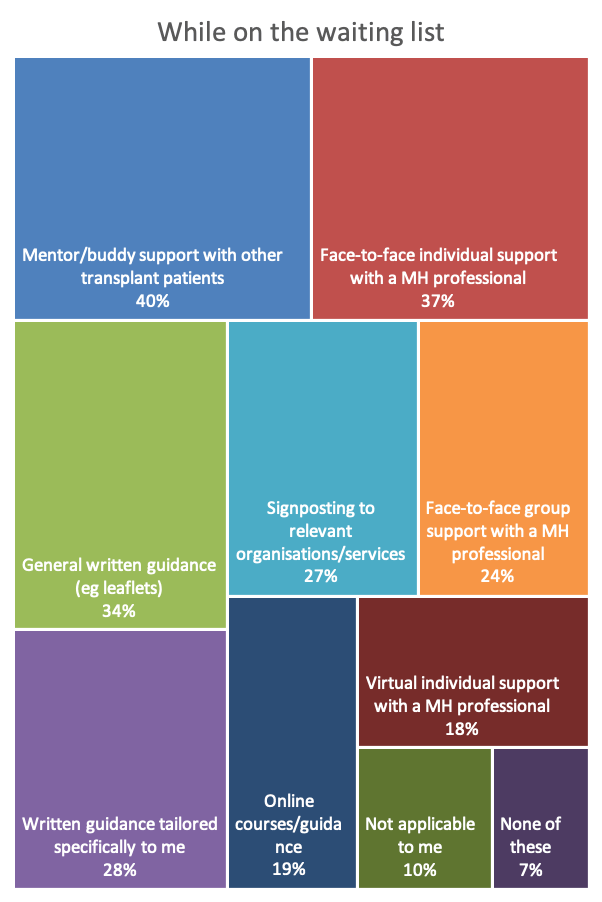
259 people answered this question.
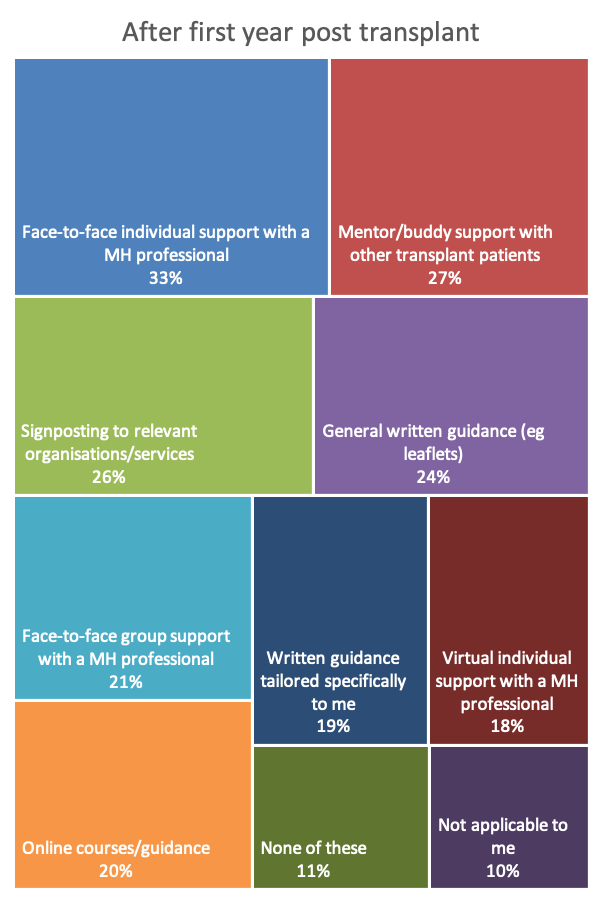
We asked the same question to people who had had transplants only, thinking about the first year after transplant. The most preferred option was face-to-face psychological support (52%), followed by mentor/buddy support (50%).
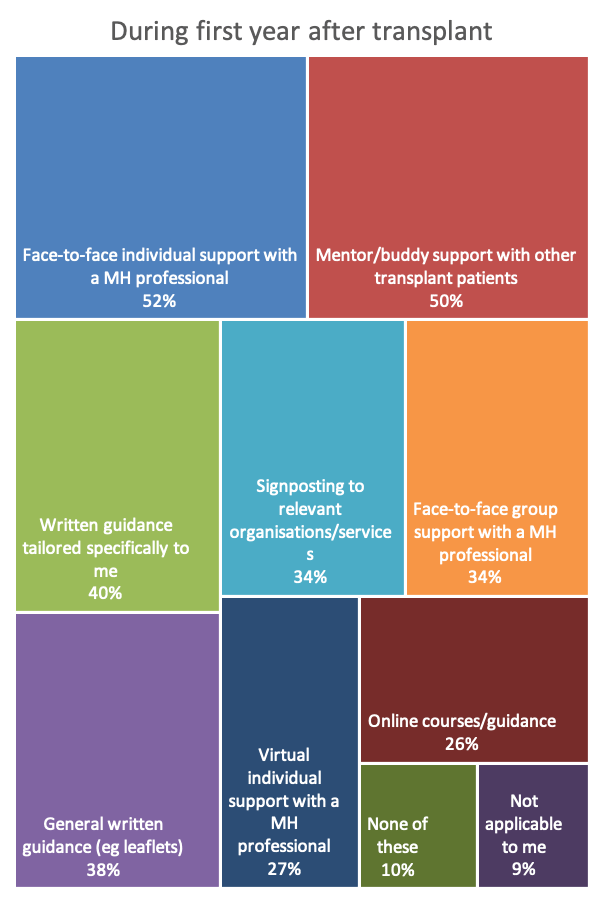
223 people answered this question.
The same question was put to people who had had transplants more than twelve months previously. Although fewer people thought it would be beneficial, the top choices continued to favour face-to-face individual support (33%), and buddy/mentor support (27%). Support from patient organisations was also picked by just under a quarter of respondents (21%).
187 people answered this question.
Mental Health Discussion
Important
It's no surprise that psychological support is needed from the very start the transplant process and continuing into the long term. The results showed that the issues and the type of support required differed between people or between the different timeframes for individuals.
Support needed
Psychological support was seen as important to patients, particularly those on the waiting list for a transplant. Respondents indicated that they needed psychological support both before and after transplant. The issues people experienced relating to mental health varied depending on the stage of their transplant journey.
On the waiting list for a transplant, respondents appear to go into ‘survival mode’ with the focus being on getting a transplant, the possibility of not getting the call in time and anxiety relating to health complications and the surgery itself. They report feeling anxious, stressed, overwhelmed and depressed (low mood).
Time spent on the waiting list creates anxiety and uncertainty – we know from experience on our online forums and patient meetings, as well as the results in this survey, that these issues can often be eased slightly by talking to others who have been in the same position. Indeed, respondents identified mentor/buddy support with other transplant patients as a beneficial source of support. Other sources included face-to-face support with a mental health professional and written materials, both tailored to the individual and general.
Complex issues
After transplant, particularly in the first year after transplant, the psychological issues appear to be more complex and far-reaching, with the added pressure of survivorship, feelings of guilt and feeling a pressure to live the best life possible in honour of and in gratitude to their donor.
Half of respondents reported feeling anxious, overwhelmed, depressed/low mood and stressed during the year after transplant, and 43% had difficulty adjusting to their new life. We saw these persist well beyond the first twelve months after transplant for around one in three respondents.
These psychological issues appear to peak months after the transplant operation. It is possible that this arises as the physical issues start to reduce and the emotional impact of what has happened start to come into focus. There is a burden of expectancy to be ‘well’ and our survey showed that some patients had difficulties coping once the focus moved away from physical healing.
There were, however, comments from people who expressed that they didn't need any help or didn't wish to seek it themselves. More research is needed to understand to what extent this relates to the pressure to be ‘positive’ and ‘well’, or true resilience.
Timely evaluations needed
We saw an interesting phenomenon in the response patterns. Fewer people who had had a transplant at least a year ago reported needing help and placed less importance on psychological issues while on the list and in the first year after transplant. A far higher proportion of people who were actually on the list or in the first year after transplant reported that psychological support was important and that they needed it. This tells us that when evaluating the needs of service-users, opinions should be sought from current patients, rather than relying on retrospective views.
We asked respondents how important it was to be given physical fitness advice before and after transplant. Overall, 84% of our respondents said that it was very or extremely important during the first twelve months after transplant. Over half said it was extremely important. A third felt it was extremely important while on the waiting list and also after the first year of transplant.
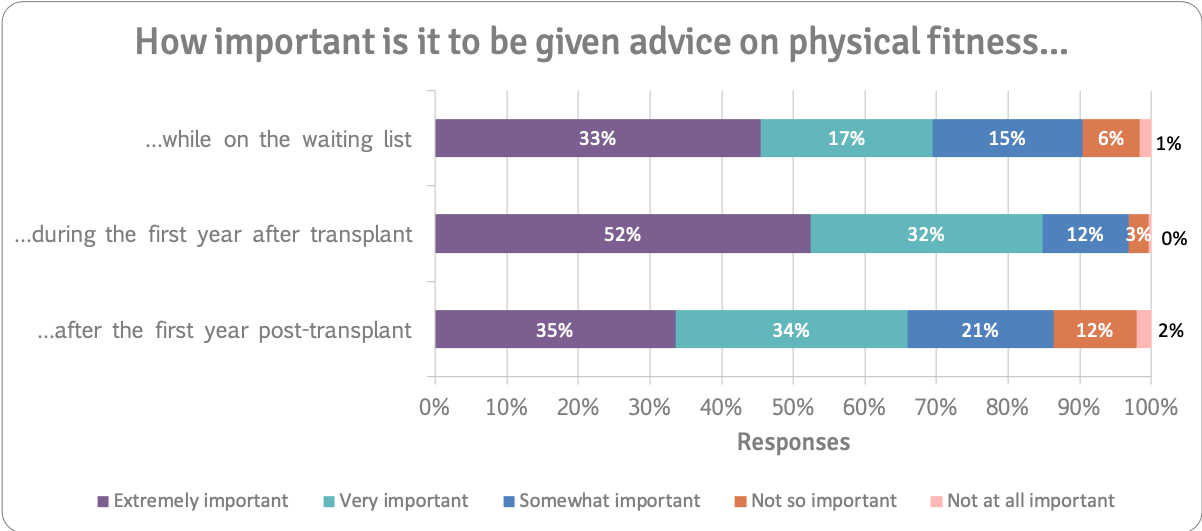
259 people answered this question.
Physical fitness support was most important to the 36 people who had had a transplant in the previous twelve months. The chart below shows responses from these people. Over half felt it was extremely important while on the waiting list, increasing to nearly three-quarters (69%) of respondents in the twelve months following transplant.
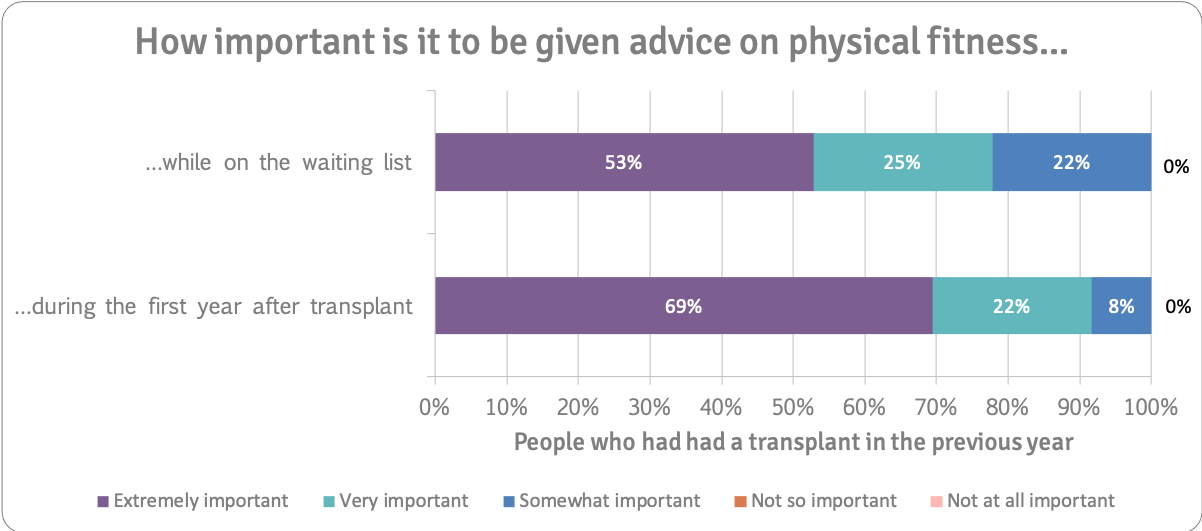
36 people answered these questions.
While on the Waiting List
We asked respondents to tell us about physical fitness problems they experienced (or were experiencing) while on the transplant list. The main problems identified were not being physically able to do exercise activities (39% ), not having the motivation (28%), and not knowing the intensity (24%) and kind (22%) of exercise that was safe. You can see the percentage of people that identified each problem on the chart:
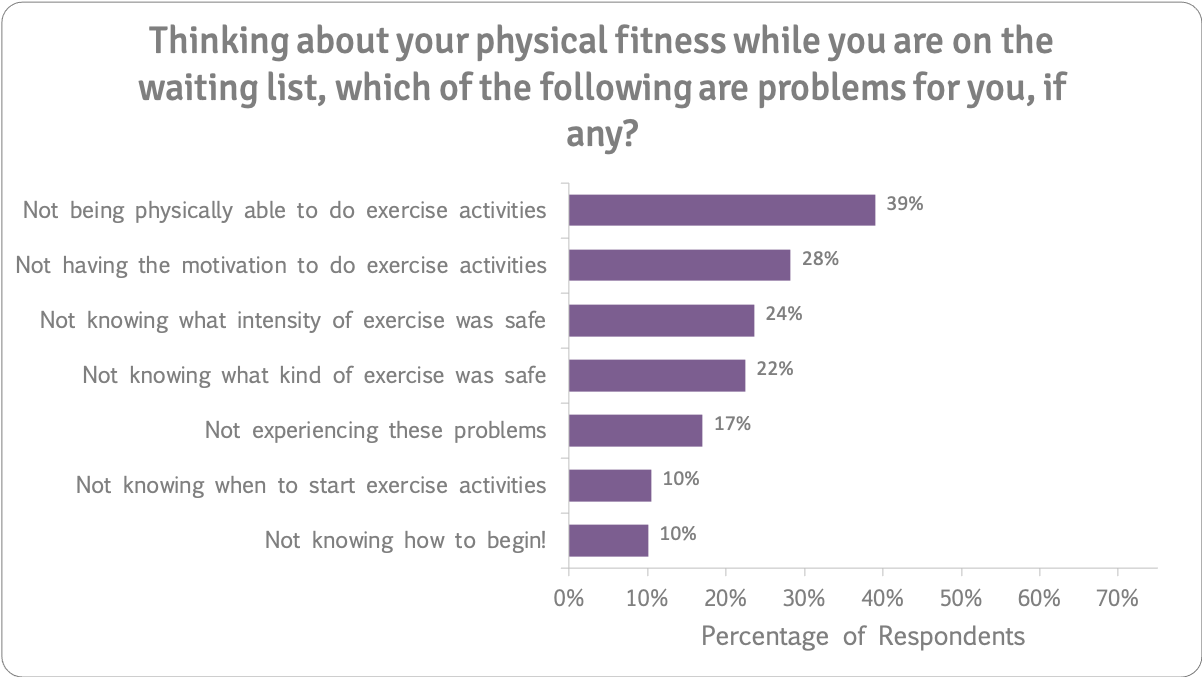
259 people answered this question.
During the First Year After Transplant
A higher proportion of respondents identified physical fitness problems during the first year after transplant than they did for the period they were on the waiting list.
Two out of every three (65%) people didn't know what intensity of exercise was safe or what kind of exercise (63%) was safe during the first year after transplant. 57% said they didn't know when to start exercise activities. 43% were not physically able to do exercise activities and 39% didn't know where to begin.
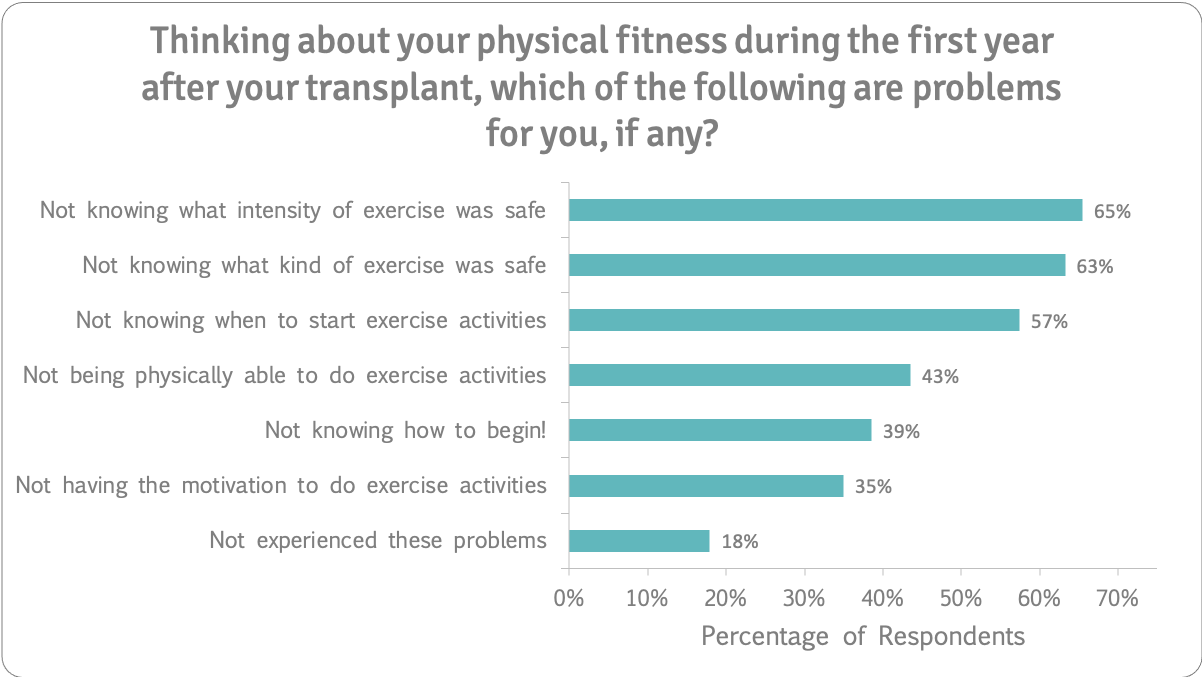
223 people answered this question.
After the First Year Post-Transplant
We asked people who had had a transplant at least a year ago what physical fitness problems they experienced after that first year after transplant.
A quarter did not experience the problems. All issues were reported less frequently for the period after the first twelve months post-transplant.
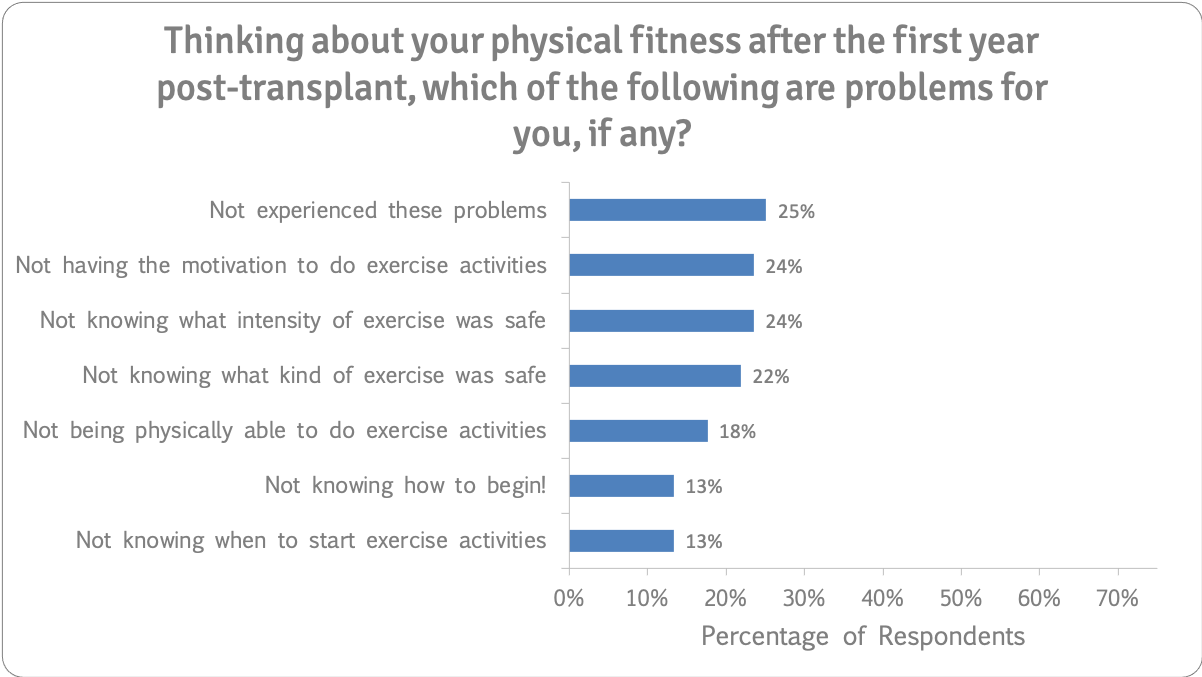
187 people answered this question.
Physical Fitness Help
We asked respondents if they felt they needed physical fitness help with these questions:
While on the waiting list, do you feel you need help to stay physically fit enough for transplantation?
During the first year after your transplant, did you feel you needed help regaining a good level of physical fitness?
After the first year post-transplant, did you feel you needed any kind of help with your physical fitness?
This chart displays a summary of what all respondents said:
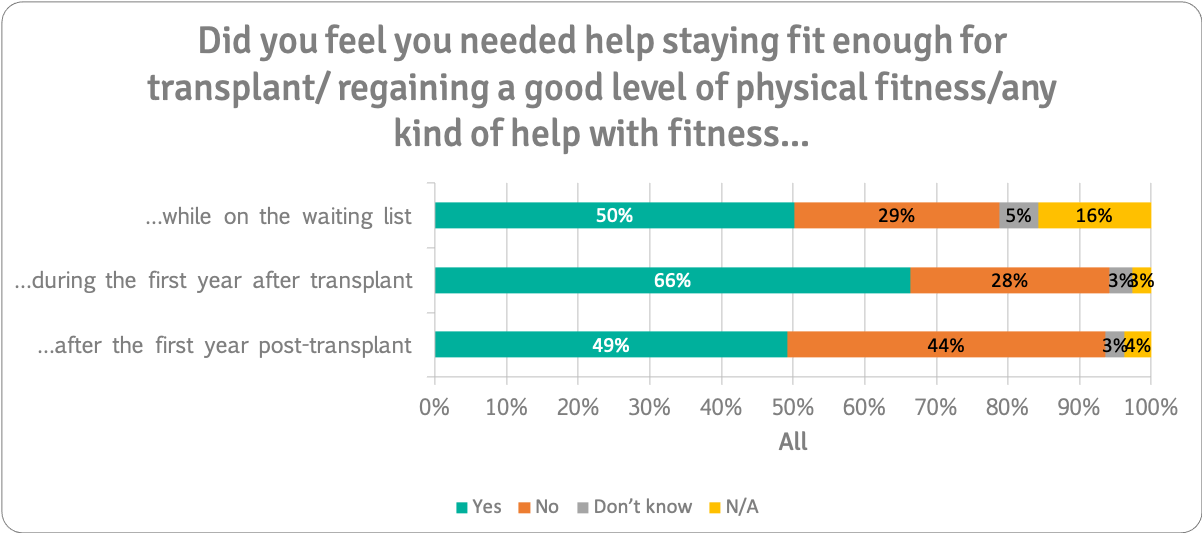
Half (50%) said they needed physical fitness help while on the waiting list and nearly two thirds (66%) said they needed it in the first year after transplant. This dropped to just under half after that first year post-transplant.
259 people answered these questions.
People on the Waiting List
Two thirds (69%) of people who were on the waiting list said they needed help to stay fit enough for transplant while on the waiting list:
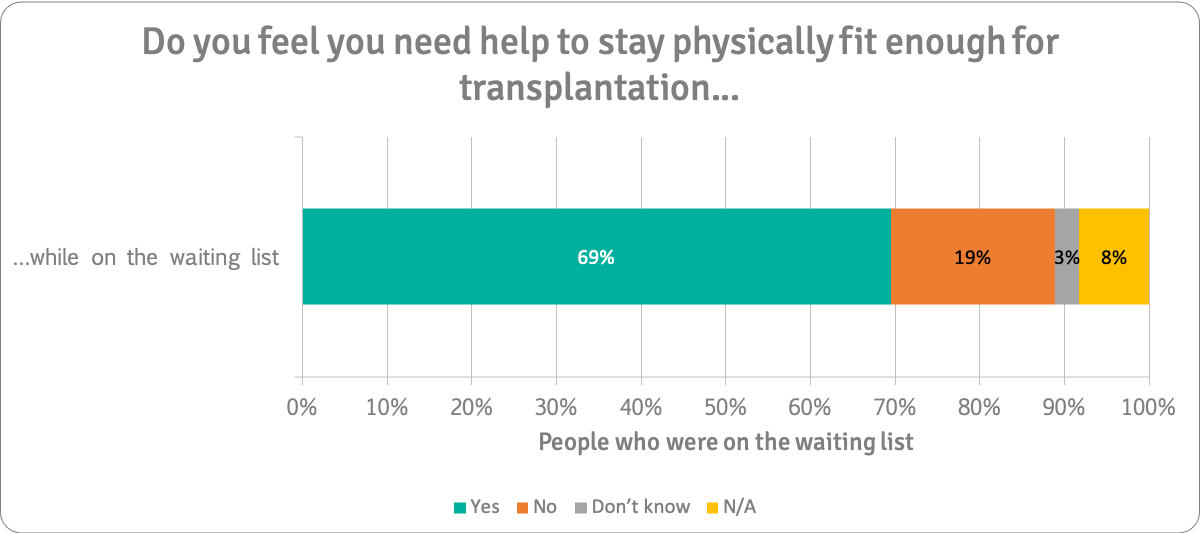
36 people answered this question.
People who had a Transplant in the Previous Year
We asked respondents who had had a transplant within the last year if they felt they needed help staying fit enough for transplant while on the waiting list and help regaining a good level of fitness during the first year after transplant.
As with psychological support, people who were actually on the waiting list at the time of the survey were more likely to say that they needed help to stay fit enough for transplant while on the waiting list (69%) than those who had already had transplants who were looking back on their time on the waiting list (56%).
Three-quarters (75%) said they needed help during the first year after their transplant to regain a good level of fitness.
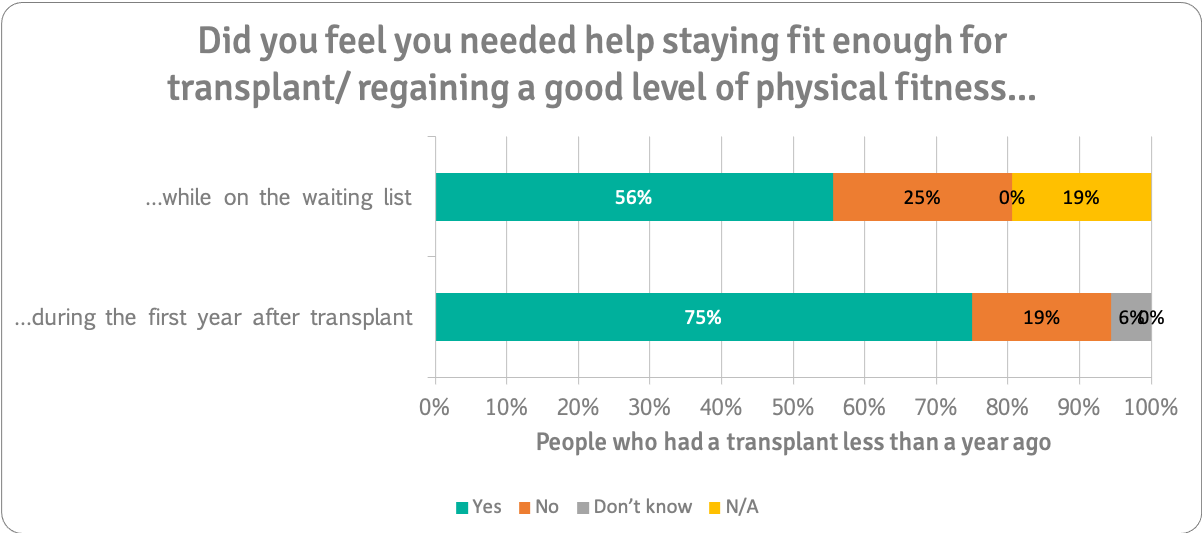
36 people answered these questions.
People who had had a Transplant at Least a Year Ago.
We asked respondents if they felt they help staying fit enough for transplant while on the waiting list, help regaining a good level of fitness during the first year after transplant or any kind of help with their physical fitness.
Note that the people on the waiting list and people who had a transplant within the last 12 months were not asked this question.
65% said they wanted help during the first year after transplant, compared to 75% (above) (who were still in their first year after transplant.
Half (49%) said they needed help with their physical fitness after the first year post-transplant.
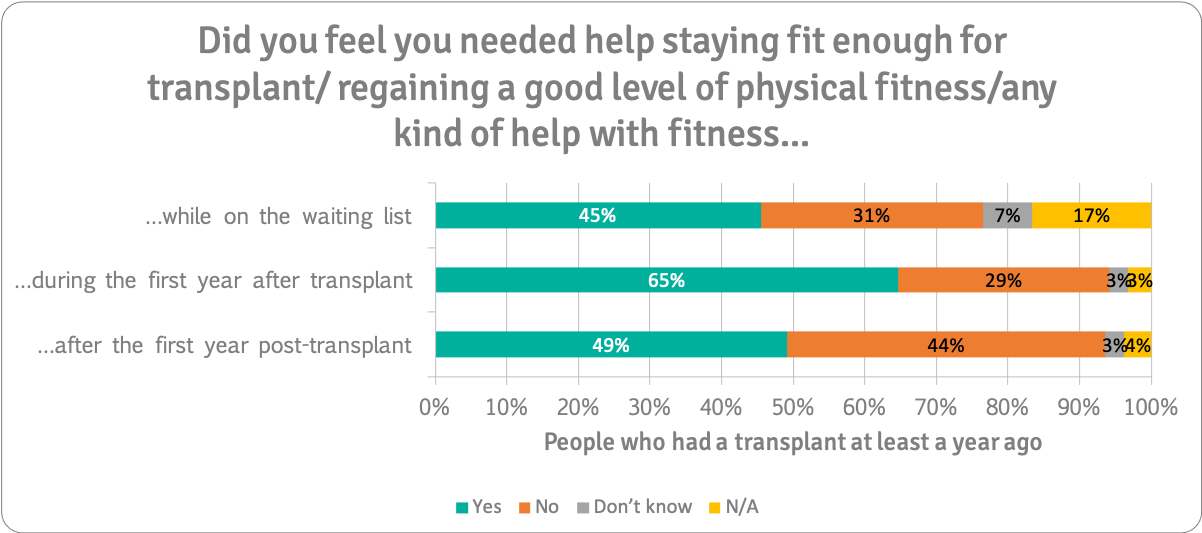
187 people answered these questions.
“Addenbrookes hospital have been great. At 9 weeks post transplant they allowed me to go to zumba but no twisting or stretching. At 16 weeks I could do more. They have always advised me and answered questions.”
“I’m still in my first year of recovery and I want to exercise as I know my physical activity isn’t what it was pre-transplant but I don’t know how to go about it, or how intense to go. I don’t want to accidentally overwork myself and cause a hernia or some further health problem. I also keep getting I’ll every time I’m ready to start exercise so it seems like I’ll never get around to it by this stage”
“It appears some folks do little or nothing, to regain fitness, while others have completely over optimistic expectations. Peoples' post transplant health also varies widely and so advice must be tailored for individuals”
“I got very limited advice mainly from physio in hospital. I went to a rehab physio privately and then to a personal trainer afterwards which was good but they were unclear themselves what a post Tx person should do”
Beneficial Physical Fitness Support
We asked respondents what kind of physical fitness help they would find beneficial before and after transplant.
We asked people to choose three types of physical fitness support that they thought would be most beneficial while on the waiting list.
The chart below shows the percentage of respondents that picked the type of support.
Overall, having general written guidance (35%), tailored written guidance (32%) and one-to-one exercise sessions (27%) were most likely to be picked.
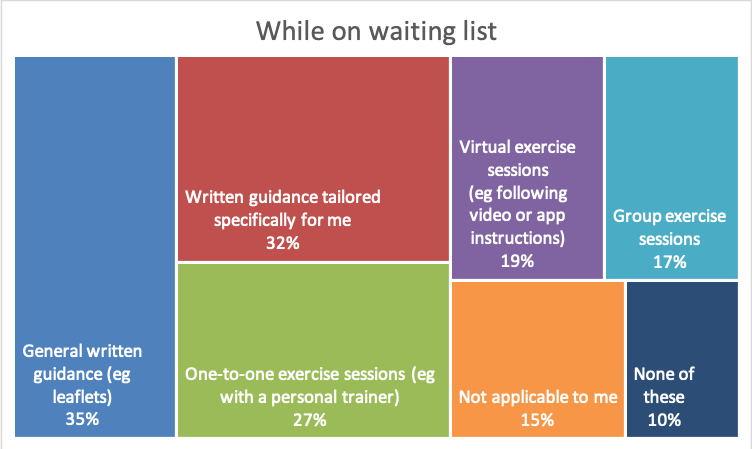
259 people answered this question.
We asked the same question about beneficial fitness support during the first year after transplant. The most preferred option during the first year after transplant was one-to-one exercise sessions (53%). Notably, a higher percentage of people picked this in the first year after transplant than they did for on the waiting list.
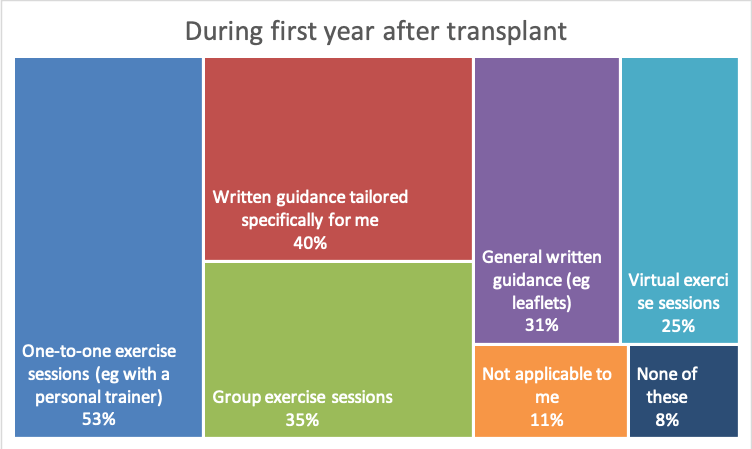
223 people answered this question.
The same question was put to people who had had transplants over twelve months ago. Fewer people chose specific types of support, but the top choices were one-to-one exercise sessions (25%), group exercise sessions (25%), tailored written guidance (20%) and general written guidance (18%).
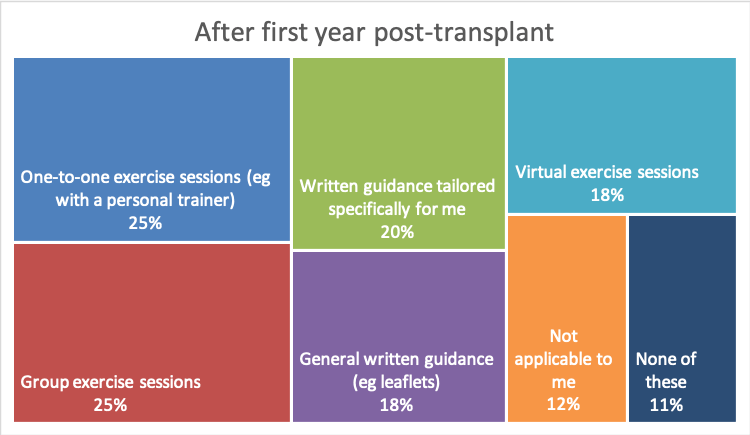
187 people answered this question.
Physical Fitness Discussion
The definition of fitness
When we talk about physical fitness and liver transplant, we are talking about being fit enough to undergo transplant surgery, or making a recovery to a level of fitness that allows you to do the things you want to do. For some this is doing daily activities around the house. For others, it is about being physically fit enough to compete at sports.
The shift to safety
While people were on the waiting list, the main problem with physical fitness was simply not feeling able to exercise. Post-transplant, the focus tends to shift to safety, and what people should and shouldn't be doing. If this isn't addressed early on, it can remain an issue for people in the long-term.
Four out of five (84%) post-transplant patients said that physical fitness advice was very or extremely important during the first twelve months after transplant. Two out of every three (65%) people who had had a transplant didn't know what intensity of exercise was safe or what kind of exercise was safe (63%) during the first year after transplant.
However, the comments demonstrate that people do want to do activities to regain their fitness levels. Two thirds (69%) of people who were on the waiting list said they needed help to stay fit enough for transplant while on the waiting list. Three-quarters (75%) said they needed help during the first year after their transplant to regain a good level of fitness.
Influence of mental health
It's likely that psychological and physical issues experienced by patients play a role in attitudes towards exercise and vice versa, for example, in terms of confidence, fear of the unknown, managing the operation scar and generally adjusting to the demands of life after transplant and resuming 'normal life'.
Individual differences
The range of individual differences is reflected in preferences expressed by respondents for personalised physical fitness advice through a variety of means: one-to-one sessions (e.g. with a personal trainer) and tailored written guidance, and some thought general written guidance and group exercise sessions would be beneficial.
We asked respondents how important it was to be given specific dietary advice before and after transplant.
Overall, 59% of our respondents overall said that it was extremely important while on the waiting list and another 24% said it was very important.
Over half (56%) said specific dietary advice was extremely important during the first year after transplant with another 29% saying it was very important.
35% said it was extremely important after the first year post-transplant.
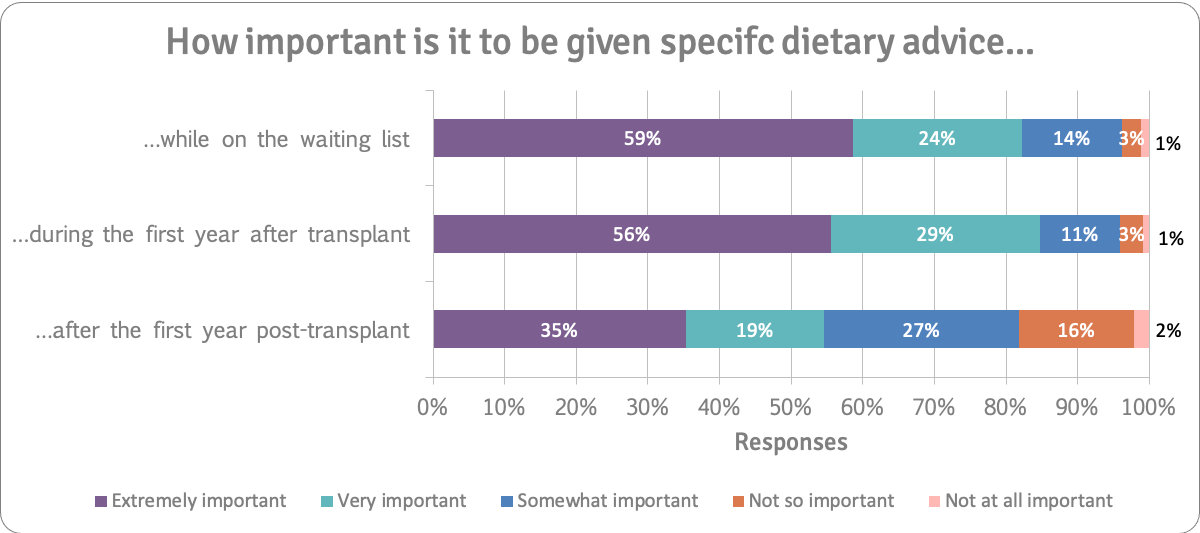
259 people answered this question.
Specific dietary advice was extremely important or very important to 91% of the 36 people who had had a transplant in the previous twelve months. The chart below shows responses from these people.
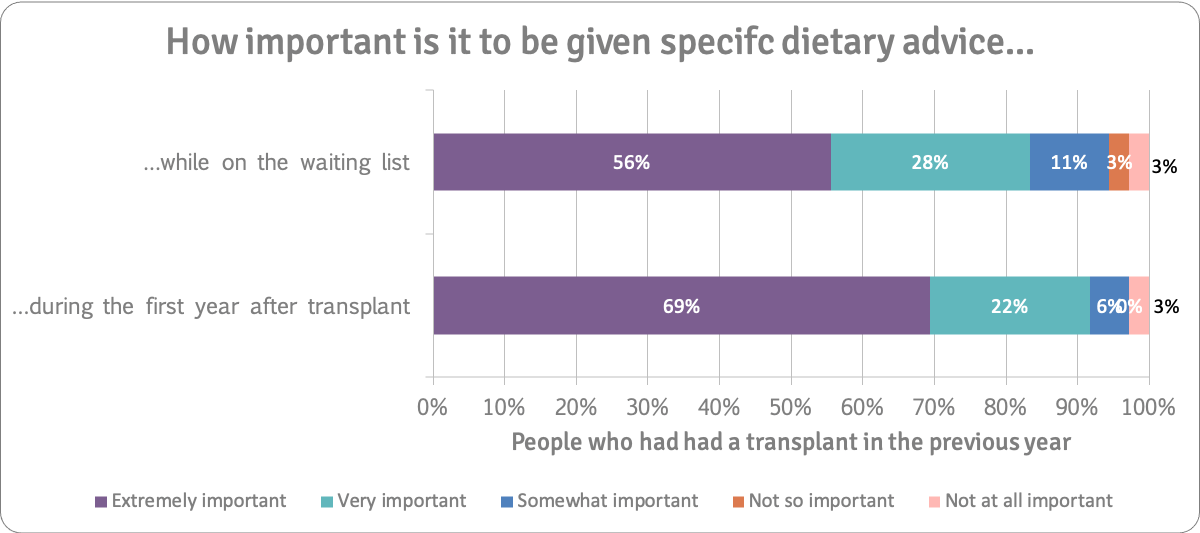
36 people answered these questions.
While on the Waiting List
We asked respondents to tell us about problems they experienced (or were experiencing) with diet while on the transplant list.
The main problems identified were not being able to eat (39% ), and not knowing how to maintain/build muscle mass (34%) while on the waiting list. Other problems for around a quarter of the respondents were around not knowing what to eat and how to get the most out of food. Not knowing how to manage weight was an issue for one in five people. You can see the percentage of people that identified each problem in the chart below:
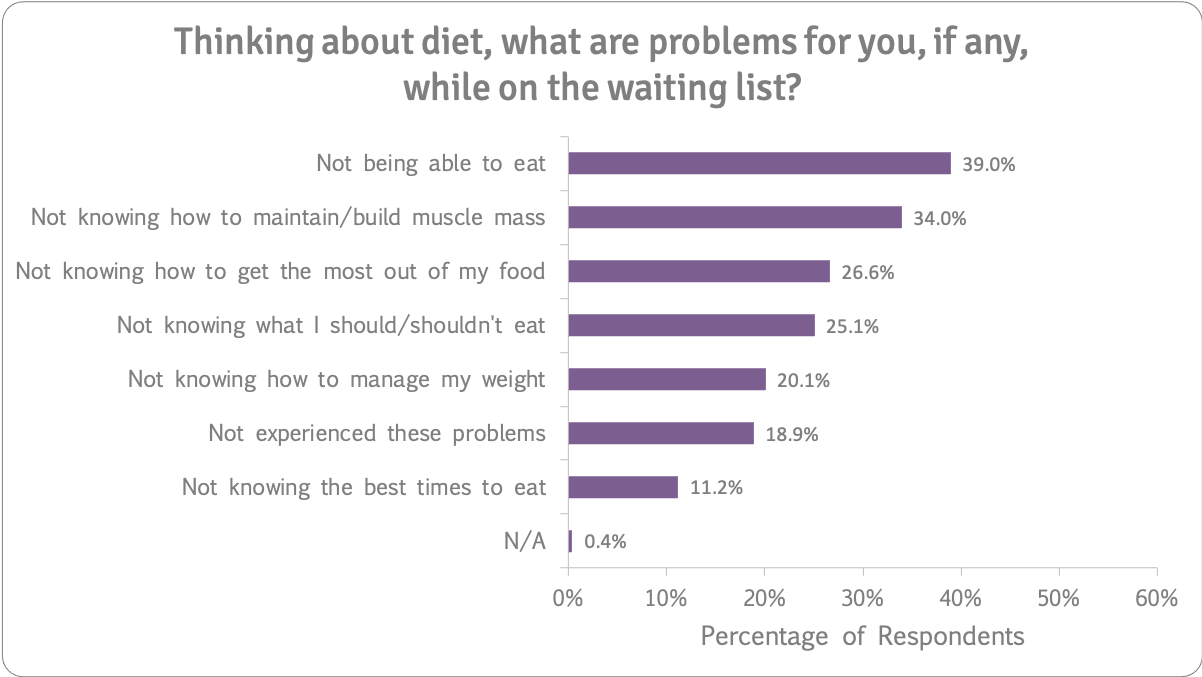
259 people answered this question.
During the First Year After Transplant
We asked people about diet problems they may have experienced during the first year after their transplant.
Just under half (45.3%) said they didn't know what they should and shouldn't eat. 43.9% didn't know how to maintain/build muscle mass. A third didn't know how to manage their weight and a quarter found not knowing how to get the most out of their food a problem. The chart below shows the responses people made when thinking about diet problems during the first year after transplant.
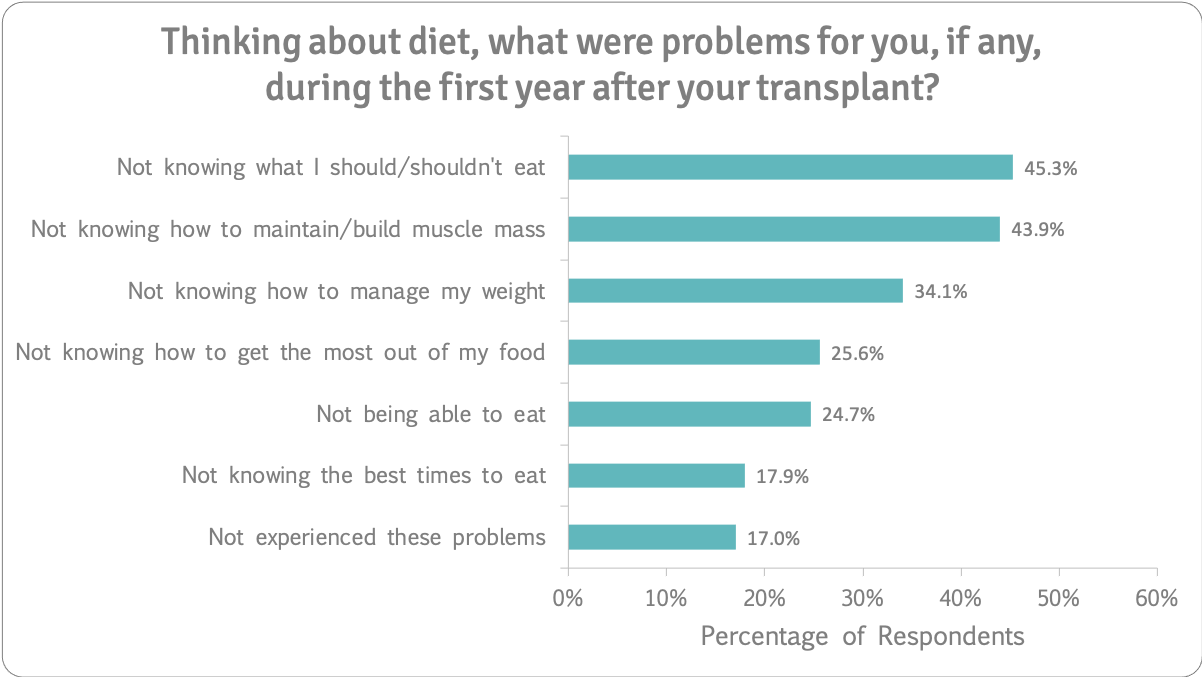
223 people answered this question.
After the First Year Post-Transplant
We asked people who had had a transplant at least a year ago what diet problems they experienced after that first year post-transplant.
Nearly a quarter (23.5%) did not experience diet problems. However 28.9% said not knowing how to manage weight was a problem.
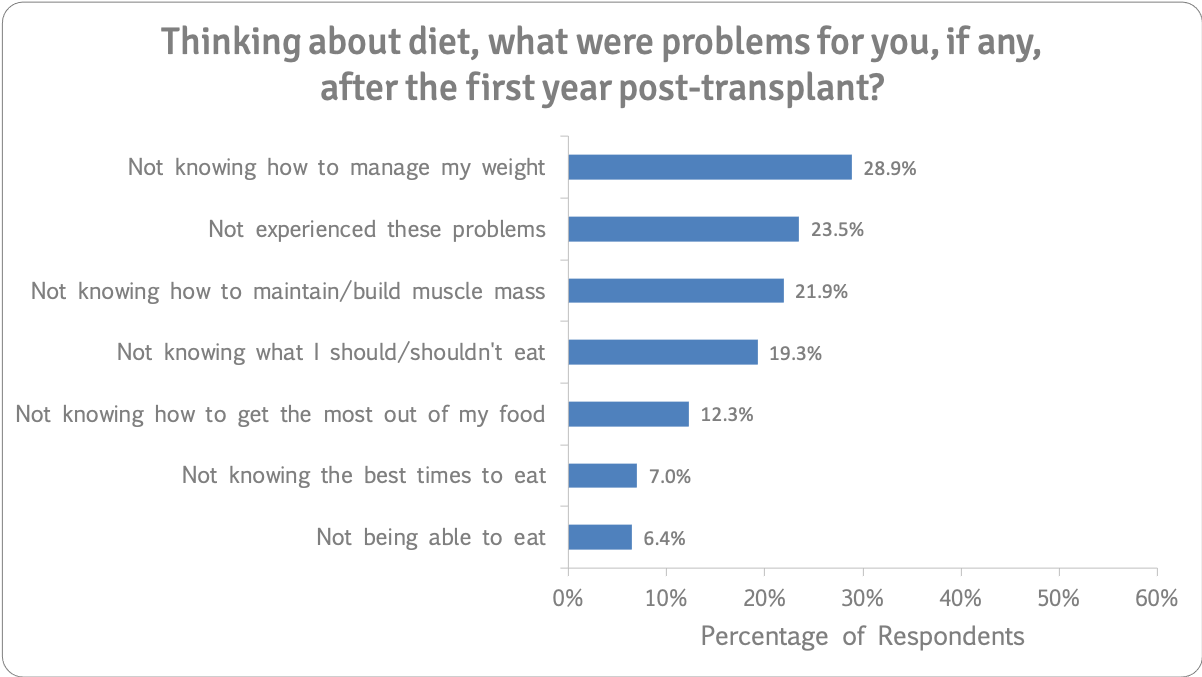
187 people answered this question.
Diet Help
We asked respondents if they felt they needed help with diet before and after transplant. 64% said they needed help while on the transplant list. Three-quarters (74%) said they needed it in the first year after transplant and still 43% said they needed diet help after the first year post-transplant.
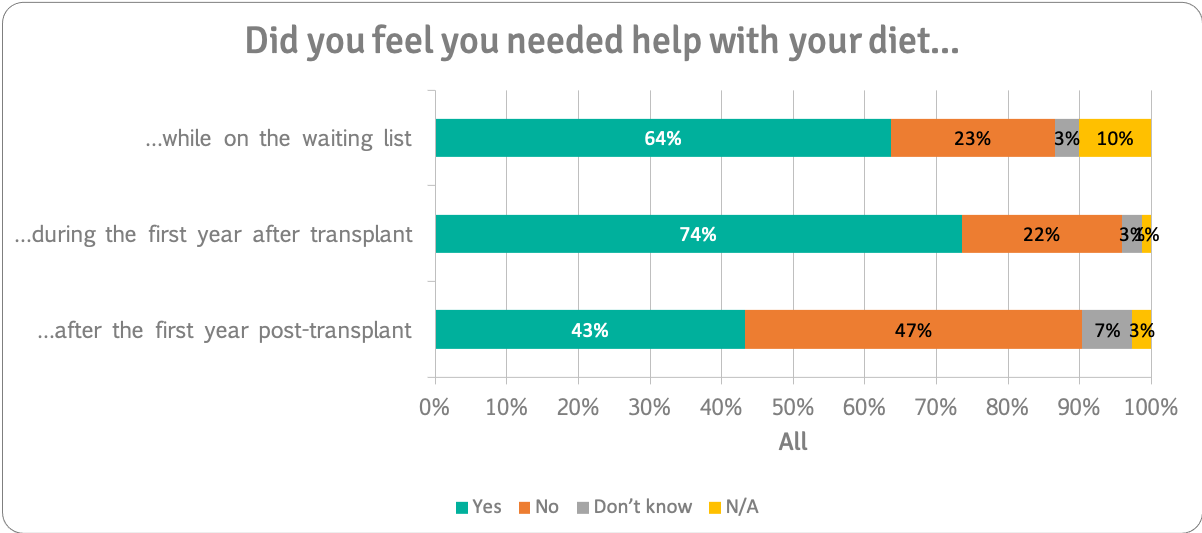
259 people answered these questions.
People on the Waiting List
81% of people who were on the waiting list said they needed help with diet.
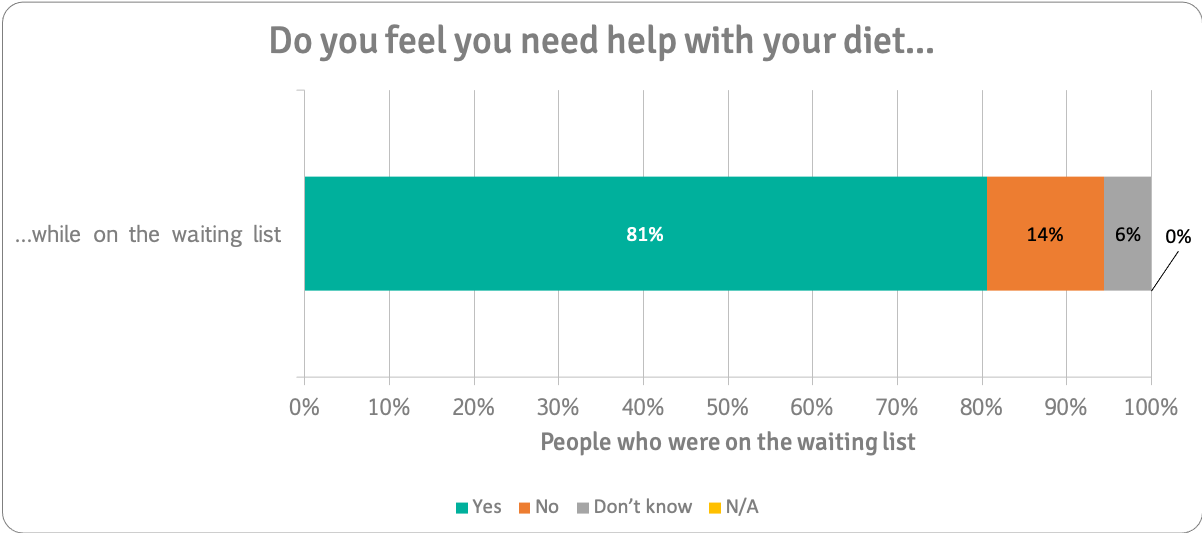
36 people answered this question.
People who had Transplant Within the Last Year
We asked respondents who had had a transplant within the last year if they felt they needed help with their diet before and after transplant.
61% said they needed it while on the transplant waiting list rising to 83% in the first year after their transplant.
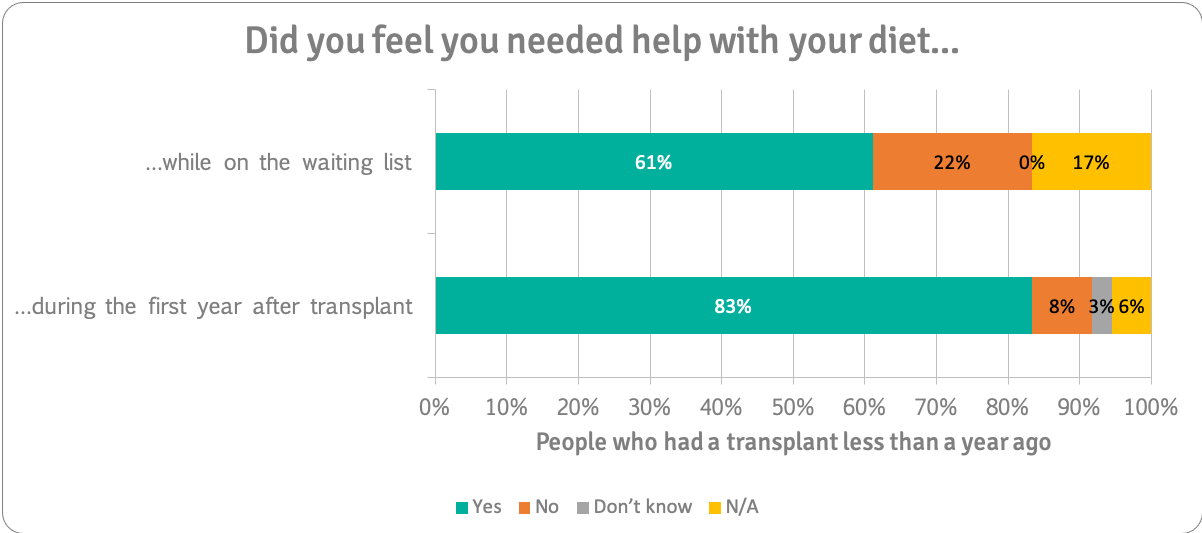
36 people answered these questions.
People who had had a Transplant at Least a Year Ago
We asked respondents if they felt they needed help with their diet before and after transplant.
61% said they needed help while on the waiting list. 72% said they needed diet help in the first year after transplant and 43% needed it after the first year post-transplant.
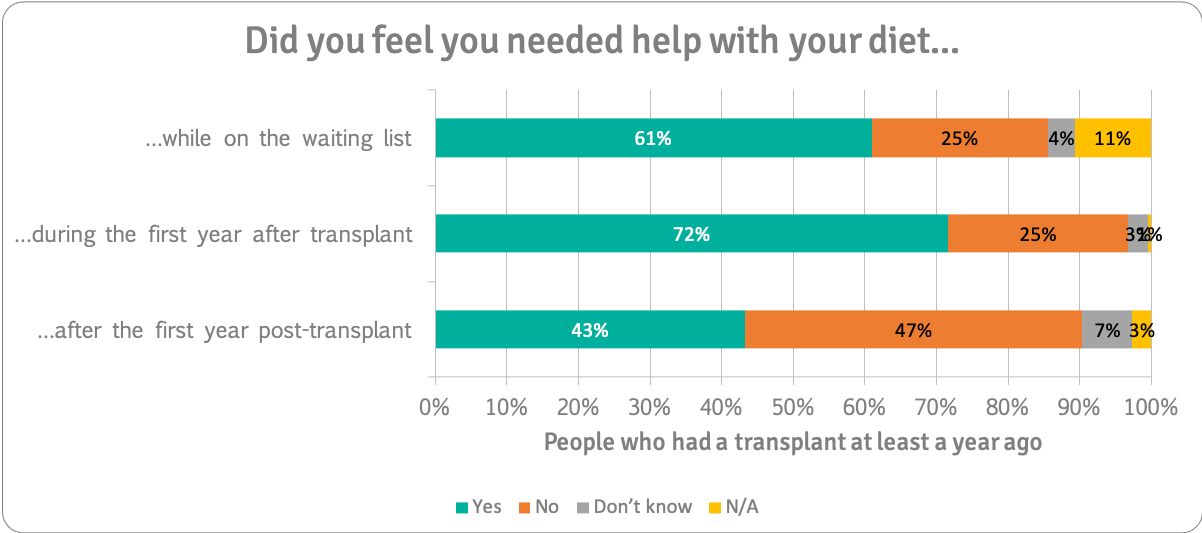
187 people answered these questions.
“The dietary support I received was exceptional. As the NAFLD progressed I was monitored closely and dietary changes made to help me. After the Op I was given encouragement and support to again readjust diet.”
“Each hospital has different dietary restrictions, this should be standardised”
“After my transplant i gained a lot of weight and struggled to get back to a health weight.”
“Colds caused appetite loss during which time I lost quite a lot of weight. My exercise routine to regain fitness ought to be tailored to diet, currently struggling with this issue.”
Diet Discussion
Diet is important
83% said specific dietary advice was extremely or very important while on the waiting list. The main problems identified were not being able to eat (39% ), and not knowing how to maintain/build muscle mass (34%) while on the waiting list.
Consistent dietary advice
85% said specific dietary advice was extremely or very important during the first year after transplant. The issues after transplant tended to be around not knowing what to eat and maintaining the appropriate weight under a new medicine regime. Historically, transplant centres have each provided their own dietary advice for transplant patients. However, more and more patients are connecting online and asking questions and comparing notes. The inconsistencies in information between centres unintentionally causes confusion about what is safe and not safe to eat.
Weight management
Some patients struggled to maintain weight whilst on the transplant list, then suddenly post-transplant started to gain weight (perhaps also being prescribed steroids).
Timely support
Where there is dietary support available, it is highly valued and welcomed, and comments reflect this. We would like to see more widely available dietary support, for all liver disease patients at all stages of their transplant journey. Ideally we'd like to see this support available from the point of diagnosis.
Did you return to or start work/education after your transplant?
We asked respondents if they returned to (or started) work/education after they had had a transplant.
Of the people who had had a transplant within the last year, 28% had done so, and 67% had not.
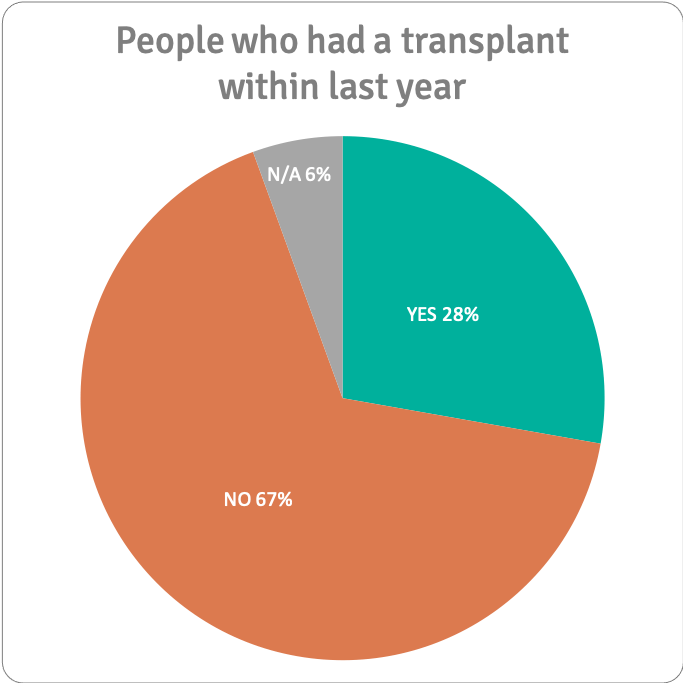
36 people answered this question.
Of the people who had had a transplant at least a year ago, 64% had started work and 27% had not.
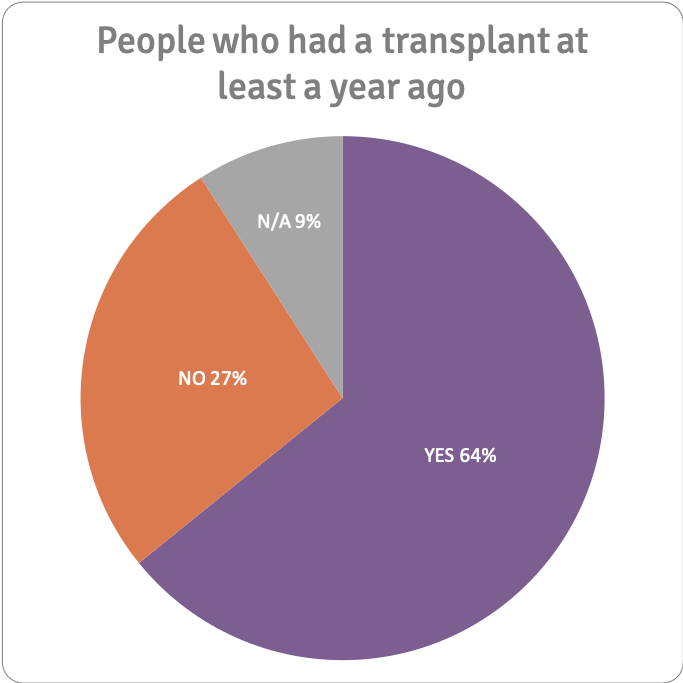
187 people answered this question.
How long after transplant did you return to or start work?
We asked people how long after their transplant did they return to or start work after transplant. 133 people gave a timescale: most returned between three and six months after their transplant.
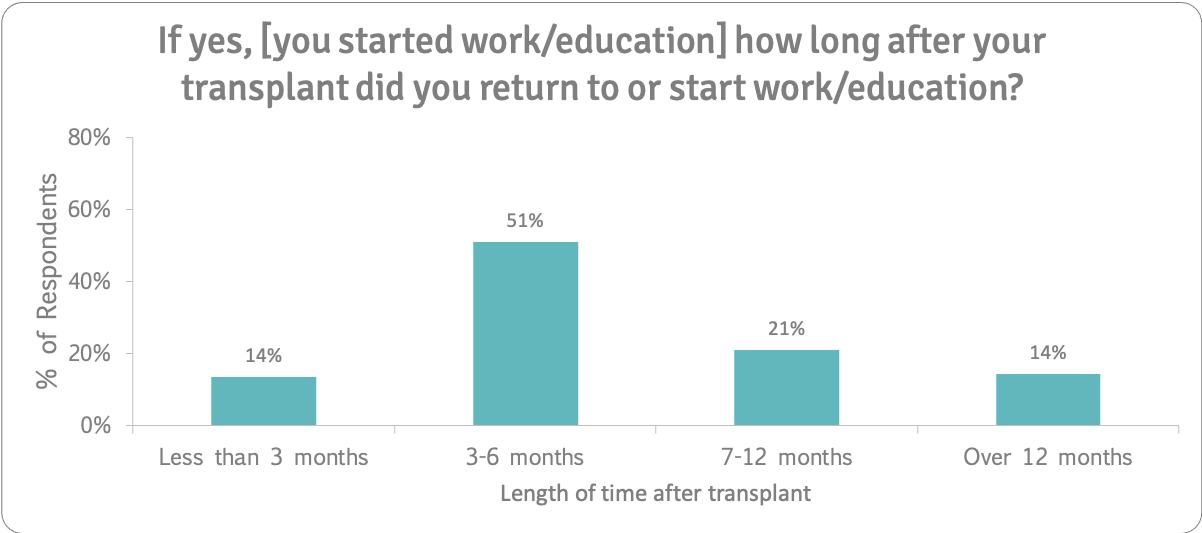
223 people answered this question (and we excluded the 90 people who ticked 'not applicable' from the above table).
Did you start at the right time for you?
Two thirds of people reported that they had started work at the right time for them. 6% felt they could have returned sooner. However 28% felt it was too soon for them.
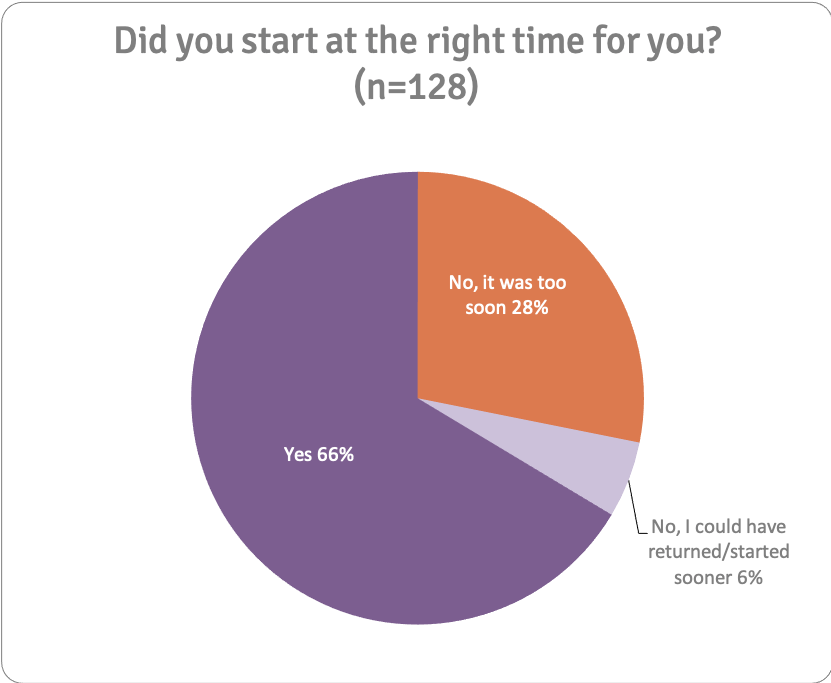
223 people answered this question. The chart excludes the people who answered 'not applicable' as this included people who had not started work. 128 people are included in the above chart.
What held you back from going to work/education when you wanted to?
We asked people, if they hadn't gone back to or started work, if there were any issues that had held them back.
The following chart shows the issues that held people back. 34% of the issues holding people back were physical ones, such as still being too ill. The other main issues were around mental health (17%), frequency of hospital appointments (16%) and lack of confidence (15%).
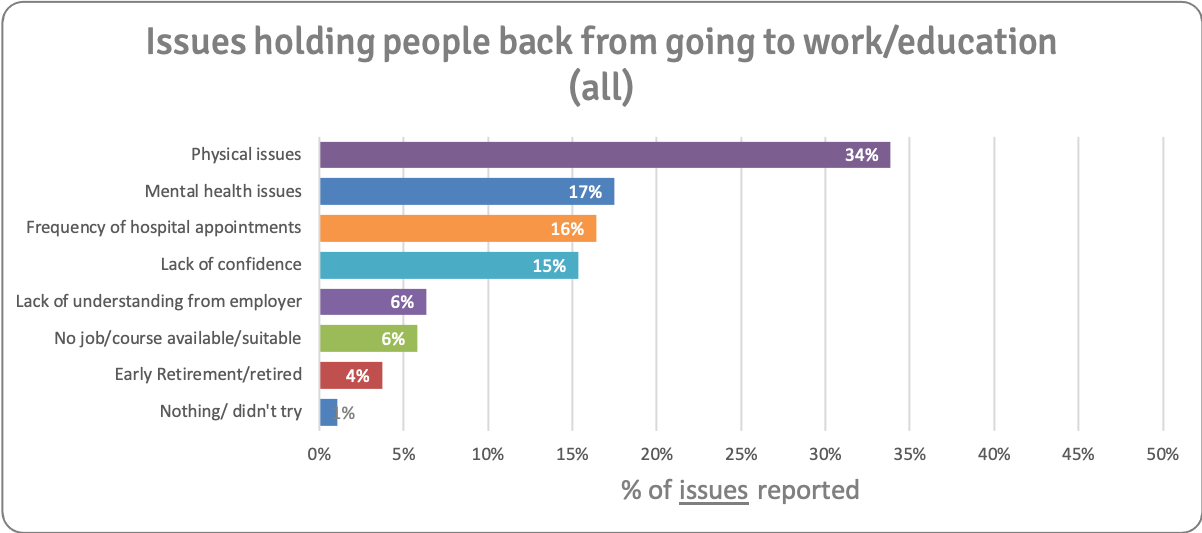
223 people answered this question, ticking 189 issues (shown in chart). 135 people ticked not applicable (e.g. because they had returned to work).
We asked respondents if they returned to or started work/education after their transplant, if they attended 35 hours a week or less, or more than 35 hours a week.
The chart below shows what hours people worked or attended education. 123 people told us whether they worked 35 hours or more/less a week. Most people (84%) started back on a part time (less than 35 hours) basis.
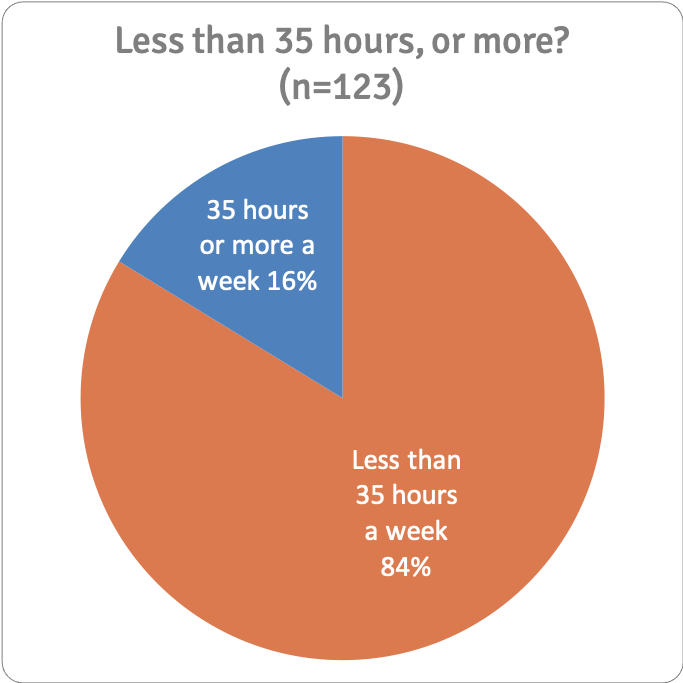
223 people answered this question (but the chart above excludes the 'not applicable' answers).
Most people were offered a phased or gradual return/start:
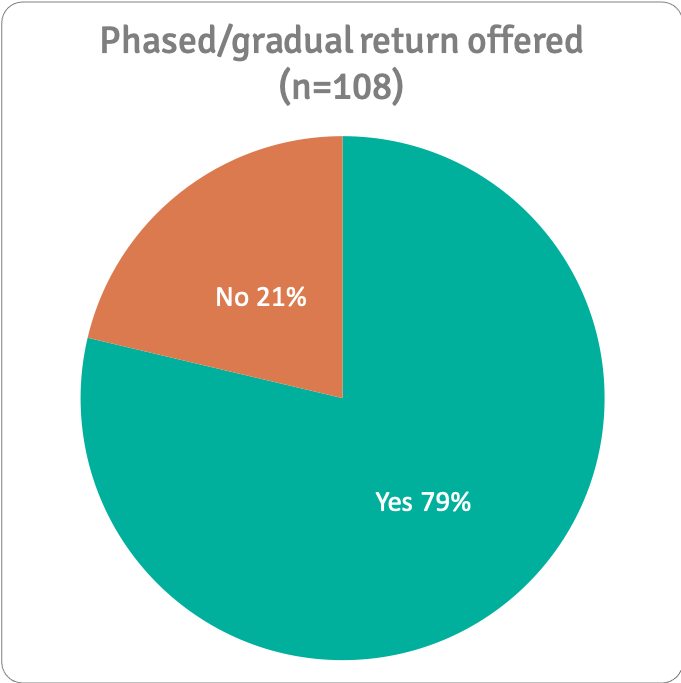
223 people answered this question (but the chart above excludes the 'not applicable' answers).
We asked people if they felt pressured to return to work. A third (32%) said they did, 39% said they did not, and 29% responded not applicable (ie had not yet returned/started work/education or did not intend to).
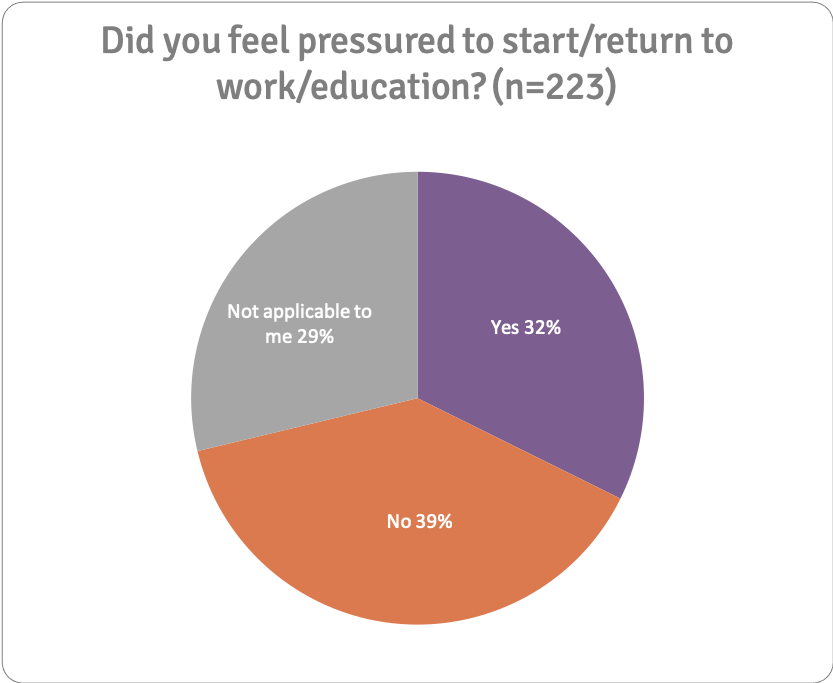
223 people answered this question.
If yes, why?
We asked those who felt pressured, why that was. Most cited financial reasons and pressure from themselves.
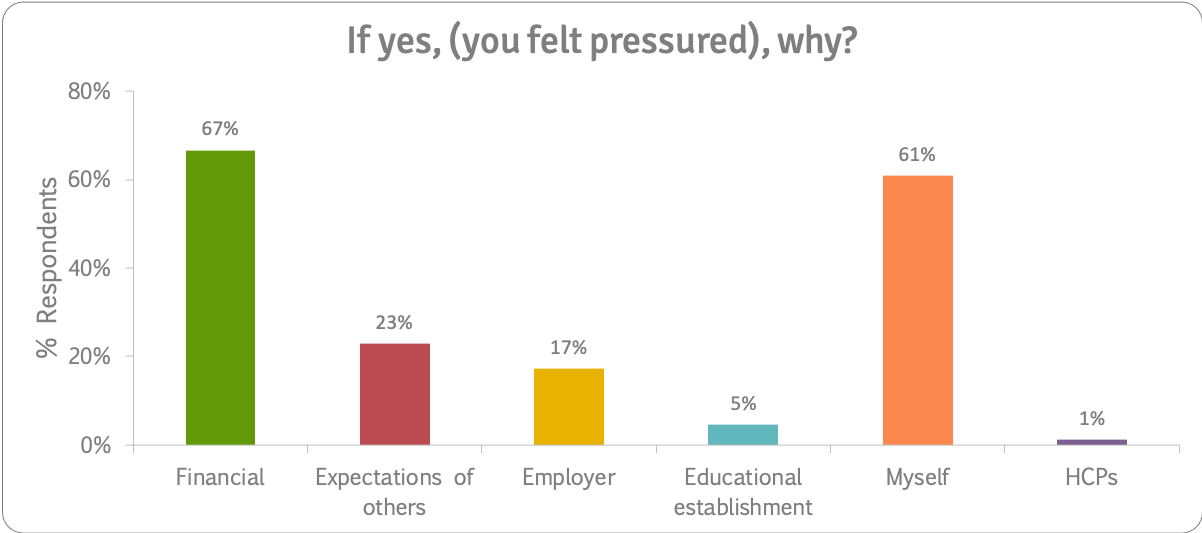
87 people answered this question.
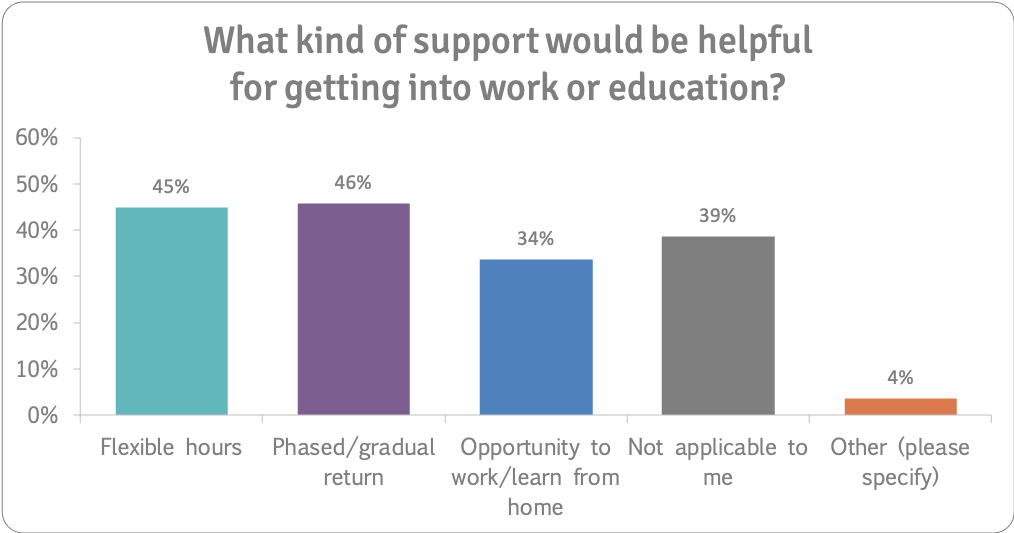
What kind of support would be helpful for getting into work or education?
Respondents said having flexible hours, having a phased or gradual return and having the opportunity to work from home would be helpful for getting back to work or education.
Other suggestions included:
“Financial support.”
“Possibility to stay on benefits while trying to see if I can safely work and support myself.”
“Employers to be informed of likely changes to personality, stress levels and potential mental issues.”
“Advice on how to attain the qualifications needed to become a counsellor.”
“Listen to the patient so his whole life isn’t ruined because of the ego of the consultants.”
“Part-time jobs.”
“Helping us to reassess what we want from life and post transplant.”
223 people answered this question.
“Still off sick and would have to look for another job which in turn I am not ready yet and the future employer would not tolerate all essential appointments or be understanding”
“I was ready emotionally and ended up going off with stress four months later
It was the right time for me in all senses except for the fact that I had a CMV infection.”
“didn't think I'd be able to get a job with my health record so didn't bother”
“Although I returned to work, I suffered from lack of confidence about being able to do my job. This lasted for about three months.”
“Had to sell our business due to illness. Then basically had to retire”
"Financial reasons, lack of financial support.”
“Yes as I'd been unwell and working from home…for a year, so had felt unreliable and that I'd had too long off work already.”
“I was told by my consultant I could go back to work so I did. In retrospect I wasn’t yet fit enough to return especially as my work only offered a two week phased return. I also put pressure on myself to go back ASAP to make the most of the gift I was given to get back to normal.”
Work and Education Discussion
Of the people who had had a transplant at least a year ago, 64% had returned to or started work/education, and 27% had not.
Most people had returned to or started work/education within 6 months of their transplant and two thirds reported that they had started work at the right time for them. 6% felt they could have returned sooner. However 28% felt it was too soon for them.
The kinds of issues that held people back from starting work were physical issues (34%), mental health issues (17%), frequency of hospital appointments (16%) and lack of confidence (15%).
A third (32%) of our respondents who had had a transplant said they felt pressured to return to work, 39% said they did not, and 29% responded not applicable (i.e. had not yet returned/started work/education or did not intend to). Most cited financial reasons (67%) and pressure from themselves (61%) for returning to work before they are physically and mentally ready.
For some, excellent support and advice is available, but this is not universal. Transplant units should be properly resourced to be able to provide specialist services to enable people who have had transplants to resume everyday activities, including work and education.
Here are some of the comments we received about lifestyle support that was provided before and after transplant:
"I had help & advice from transplant nurses & social workers about weight maintenance & financial support"
"I have seen both specialist dieticians and physiotherapists to support my diet and physical fitness. I have also seen regular specialist doctors who support with my medical care."
"I have been given lots of help from the dietitian. The education session at Kings was helpful at giving advice about diet and exercise. Questions do sometimes arise and it’s hard to know where to turn to with these minor questions."
"A few months after having my transplant, I met with a transplant coordinator and she helped me to understand certain things about growing up and my future after a transplant. I found this talk really helpful but I think it should’ve been had a few months before I ended up having it."
"Fantastic advice on everything from kings, both face to face, group sessions and comprehensive written booklets"
"None, felt extremely let down by my consultant."
"Support from a over loaded social worker "
"At regular check ups but no ongoing reference materials for between check ups which would be helpful"
"Dietitian and brief chat about mental state."
"Booklets only"
"I had the most amazing liver transplant coordinator "
"Can’t remember any except no alcohol and lots of bits of paper - disjointed - about what not to eat."
"I had help & advice from transplant nurses & social workers about weight maintenance & financial support "
"I was given the standard dietary advice but it needed more specific tailoring to my needs."
"Only exercise advice and help from the renal department"
"I can’t speak highly enough about the professional expertise and advice I’ve experienced since my NAFLD diagnosis. The people were superb and I can never repay their kindness."
"I was given a few leaflets and verbal advice whilst in hospital after transplant but had nothing since. I had my transplant 18 years ago so hoping things have change since "
"None"
"One dietitian appointment pre and one post transplant."
Here are some of the comments we received about healthcare and liver transplant:
"government bodies not understanding how my illness affects me .Having to cancel plans last minute due to being unwell and having never been unwell until you get struck down with a debilitating illness and finding yourself unfit for work"
"I think sometimes I need someone to check in with me, just for reassurance that I haven't been forgotten. Meetings with liver specialists are very clinical."
"The hospital are extremely good, and I feel able to access information or face to face appointments very quickly when needed. My GP practice, in contrast does not provide a level of support I require. I worry about the post transplant health care I will receive "
"Hepatopulmonary Syndrome is still a rarer liver disease. Unless speaking to the right professionals / physios, it can be overwhelming to cope with independently. Without the support I receive from the hospitals I am linked to, I wouldn’t be able to handle this HPS like I do."
"Most challenging thing was not wasting away and staying well enough to survive the transplant. Due to ascites I couldn't eat a lot of my regular diet, so I had a battle to maintain any muscle mass without aggravating the ascites and requiring draining which was probably the toughest symptom I had."
"Follow up care was extremely good and frequent. Now 4.5 years post transplant, appointments are much less regular. I know this is because I am well and priority is for patients are unwell, but I feel slightly less secure. "
"Lack of psychological support is my major take away. A transplant is a massive thing to come to terms with and the mental side of things is currently neglected "
"Cannot fault the care l received before and after transplant, more information could have been given about support groups before transplant and after."
"Transplant hospital was too far from regional hospital"
"I've had excellent treatment both before and after transplant. If I've had any questions or problems I've contacted my Liver Unit."
"Mental health/psychological support was something I felt I desperately needd but kings did not offer this. Going through the whole listing process and waiting process is tough, an emotional rollercoaster I felt unprepared for and would have really valued having the opportunity to talk to someone at my regular clinic appointments, someone who understood the process, pressures, concerns and questions I had about my future and the transplant."
"Nobody seems to know how to advise people who want to be really fit and active post transplant. All the advice is tailored to the old and sick and I felt I had to make it up as I went along"
"I definitely feel there needs to be more psychological help immediately after and within the first year of transplant, as personally I found this time the most difficult and did not have any care in this area. "
"First class care at Edinburgh Royal"
"I don’t feel there is enough emphasis on mental health. I appreciate my team might have been assessing my mental health through their observations etc but I was never directly asked how I was coping mentally "
"The team at the QE have been amazing! Whilst going through the transplant assessment I was admitted, which meant I had daily contact with everyone and by comparison it can now seem a bit daunting to have come home and be just waiting. I know they are all at the end of the line and that I will be seen in clinic, but there could be more self-support offered, such as online material or a weekly email/telephone call to the patient just to check in (optional) "
"Transplant team at the Freeman Hospital are excellent and provide emotional, physical and psychological support not just to me but to my family"
"Transplant Co-ordinators are AMAZING!!!"
"My post transplant experience has not been good, heamtoma, persistent constipation, serious mental health issues which I did not have pre-transplant, complete rejection. I have not always felt listened to and there is an overfocus on 'the numbers'. My mental health presentation was subtle at first but progressed significantly. No one listened to me, or my partner. By time anyone took anynotice I was acutely psychotic requring ECT, and anti-psychotics. I believe teh lack of any specialist mental health transplant expertise in England, and the lack of any MH provision as an essential element of the transplant pathway contrinuted significantly alongside the lack of any cross NHS boundary pathways for transplant patients. Cross boundary working between a specialist centre and local NHS providers must be achieved otherwise patients with complications that are not purely liver focused fall between stolls as I have done. [sic]"
"I can not fault the quality of healthcare given to me by both York hospital and St James both excellent."
"I found the side effects of the drugs very difficult to deal with especially as I had very little warning of what was to come - major hair loss, constant UTIs, etc. Also I found it difficult to deal with the PTSD side of things - 7 months on these are still difficulties particularly as it all happened in the space of 2 weeks and so I was not able to process it until some months after. "
"Being so poorly that I had to give up work and so did my wife to care for me as I was so ill, loosing our house due to lack of financial support and fighting the benefits system, the whole situation has been traumatic, being told you’ve only got 6/12 months to live and loosing your home and every pressure that brings, fighting of debtors whilst being so ill, total lack of support or understanding of your situation, suffering from depression as your world has been turned upside down. Not knowing where to access help or what help is available."
"Pre transplant is a horrible experience, those around you see you deteriorate with nothing they can do to help. I was keen to stay active and give myself the best chance of remaining healthy but this is something I took on personally, I have seen others suffer who become patients instead of fighters. "
"After transplant it would be nice to have one post transplant nurse u can contact for anything. It almost feels like your forgotten about"
"At the QE it was amazing they explained every procedure to me and my family .... and gave results of every test "
"Zero support from transplant nurses following transplant. Repatriated 300+ miles to my local hospital in a taxi after 10 days. Who was responsible for my care during this time? No pain meds given, no bed available when I got there. very poor planning and co-ordination."
"Abandoned after leaving hospital after transplant....had to find support and do own research"
"The biggest issue for me was not being told that I may suffer feelings of guilt, low mood, suicidal thoughts. I think the only thing that had kept me from committing suicide is the debt I owe to the donors family."
"I felt very isolated when I was on the transplant list. The hospital and staff were very kind and supportive but I had no idea what to expect and I felt that people made assumptions about how I felt and what I wanted. I suppose I’d not experienced or witnessed anyone who had a transplant but to the hospital and it’s staff I was just another patient. That isn’t a criticism. I think that if I’d met a transplantee it would have felt more like reality and very much more possible."
"The care my son got was second to none he is very complicated and had a real tough journey returning to theatre another 6 times in 11 weeks after transplant so our healthcare was nothing short of amazing "
"I think it is very difficult when you live so far away from your transplant unit to get any day to day week to week support. More robust liaising with local services would be good"
"Clinic follow up appointments have been exceptional. Psychological support at the transplant centre was unavailable after transplant due to demand from pre transplant patients. Referred my self to the NHS wellbeing service at 2 years post transplant. Waiting for counselling."
"My comments are really post transplant care. I am now 7 years out and attend the regional centre where I had my Tx annually and am seen locally in between. The detailed care I get at the main centre (my annual review) is much more thorough and “inclusive” of me than at the peripheral clinics I attend. One example is I get a copy of my results from the Tx centre on my annual review whereas my other BC check ups it’s no news is good news ( they only contact you if a problem. I want to feel “empowered” and feel included in my care as I take great pride in trying to look after myself to keep my results good. I would like to receive info about my BC results from ALL clinics. I do log onto GP site to access my letter from peripheral clinic but they just say FBC normal whereas annual review BC broken down into ALT etc - much more detailed. "
"As years go by with changes of staff you just feel like a number at the end of the day. Then get used to someone then they go. "
"After there was no support, especially when the transplant nurses had you back to the consultant "
"I felt that between appointments (usually once monthly) that I was very much alone in dealing with my illness while on the waiting list. Also between appointments post transplant. "
"I couldn't have had better care whilst on the waiting list or after care, however, I developed steroid induced diabetes & felt quite abandoned after hospital discharge as I was told they only took care of inpatients. After discussing this with my GP he felt I was too complicated a case so then had to be referred to the diabetes clinic at North Tyneside Hospital, delaying vital support for a condition I was very anxious about. "
"I can not fault the care and attention I received from all of the medical team as regards my actual transplant, but I was totally unprepared for the feelings and emotions I was to experience post transplant and I don't think I ever will be totally over them, and I honestly believe that more should have been done to prepare me for those feelings."
"They don’t listen they think they are Gods who know best and are not remotely interested in the patience life and how it affects them. Even after the transplant they lied constantly never explained and gave me the worst experience you could imagine. I wish I was dead "
"After transplant I felt weak. Although I asked for help to alleviate this, none was forthcoming. Now that weakness is much worse meaning that I have very limited mobility. "
"I desperately needed psychological help I didn't get any. "
"Mental health support is severely lacking"
"I was so unwell before transplant than no help may have done any good.
The feeling of guilt and shame is high after having transplant. "
"Found the lack of support for the mental side of recovery is terrible. It has taken 5yrs to finally get support for the ptsd from my transplant"
"I think I really would have benefitted from some ‘prehabilitation’ during my long wait, made up of psychological sessions and assessment of my mental state as well as healthcare advice "
"I couldn’t eat for quite some time and that was a worry."
PSC Support Prehabilitation and Rehabilitation in UK Liver Transplant Services Survey was written by PSC Support and published 11 March 2020. www.pscsupport.org.uk/transplant-services-report
Page last updated: 11 March 2020


 Recommendations
Recommendations